Researchers at the Royal Orthopaedic Hospital secure funding to develop cancer-killing injectable paste for bone tumours
The Dubrowsky Lab at the Royal Orthopaedic Hospital has secured a £110k grant to develop an injectable paste with anticancer and bone regenerative properties.
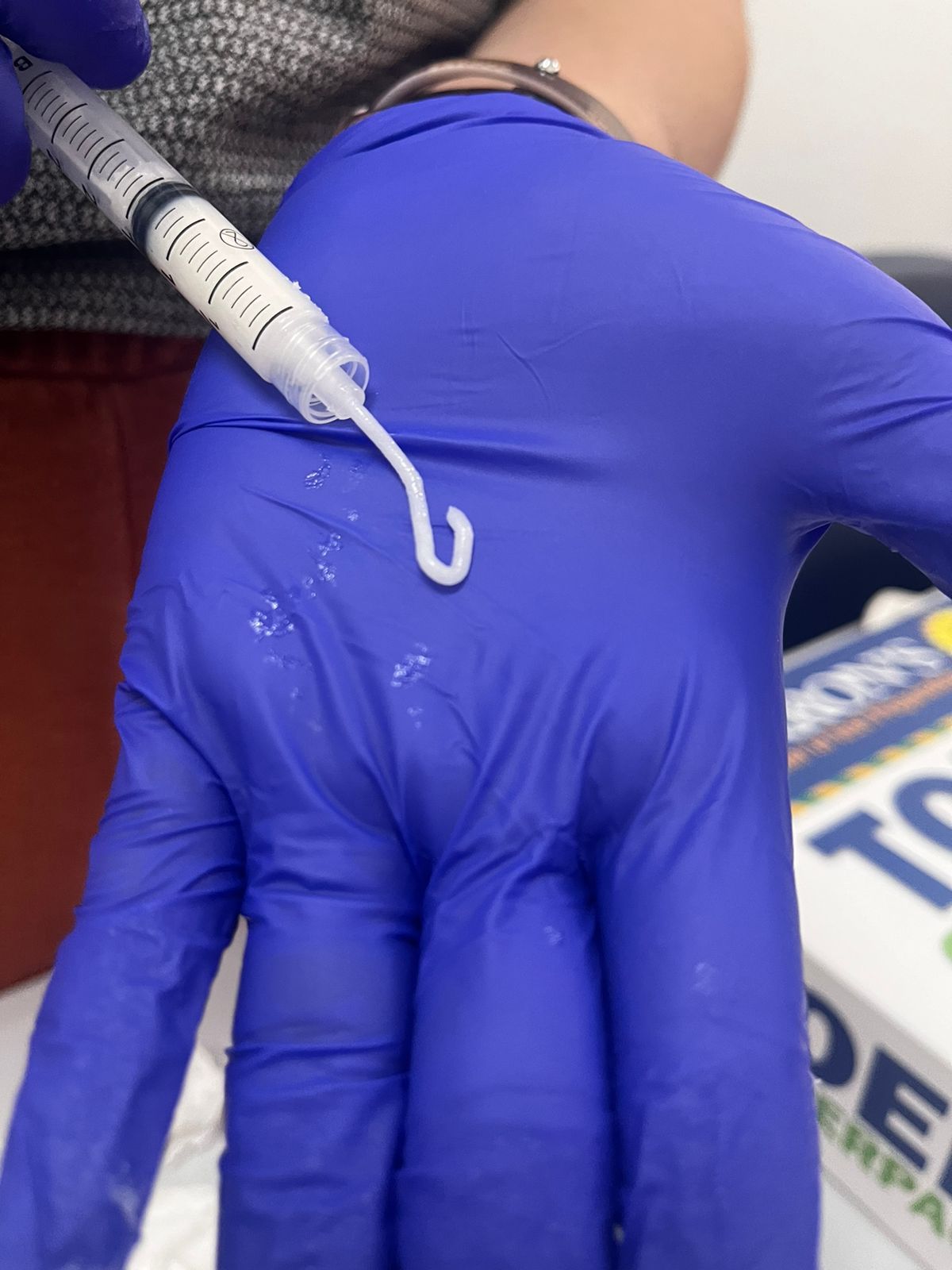
The project will see researchers at the Royal Orthopaedic Hospital (ROH) produce an injectable paste comprised of gallium-doped bioglass that if proved effective could be used to treat patients with primary and metastatic bone cancer.
Dr Lucas Souza, Research Lab Manager at the Dubrowsky Lab – Royal Orthopaedic Hospital and Lead Researcher for this new project, comments: “Advances in treatment of bone cancer have reached a plateau over the past 40 years, in part due to a lack of research studies into treatments and the complexity and challenges that come with treating bone tumours. Innovative and effective therapeutic approaches are needed and this grant from Orthopaedic Research UK provides vital funds for us to continue our research into the use of gallium-doped bioglass in the treatment of bone cancer.”
Gallium is a metallic chemical element that has cancer-killing properties. When combined with bioactive glass (used in surgeries for bone tumours to stimulate new bone growth), the material can kill cancer cells that remain when a tumour is removed and promote rapid bone formation in the area. In addition, the material also prevents bacterial contamination in the surgical site. A recent study led by Aston University in collaboration with the ROH found that bioactive glasses doped with the metal have a 99 percent success rate of eliminating cancerous cells.
The injectable paste will be particularly useful in cases of bone tumours where complete tumour removal is either not possible or not recommended. This could be for a number of reasons, such as when bone tumours are located near vital organs or because the removed tumour doesn’t have enough normal tissue surrounding it suggesting cancer cells may remain (this is called surgical margins). Injecting this paste by a minimally invasive procedure also offers a great solution in cases of benign but aggressive tumours and bone metastases where the harm inflicted by a large surgical procedure may be greater than its benefits.
Dr Lucas Souza adds: “The proposed biomaterial has the potential to drastically improve treatment outcomes of bone tumour patients by reducing cancer re-occurrence, implant-site infection rates, and implant failure rates leading to reduced time in hospital beds, less use of antibiotics, and fewer revision surgeries. Taken together, these benefits could improve survival rates, functionality and quality of life of bone cancer patients.”
The new biomaterial could also be used in combination with minimally invasive interventional therapies such as cryoablation or radiofrequency ablation. Cryoablation is a way of treating bone tumours by cooling and heating them with special needles which kills the cancer cells while radiofrequency ablation achieves similar results by using radiowaves to generate heat which kills cancer cells in bone tumours.
Dr Lucas Souza will be supported by Professor Adrian Gardner, Director of Research and Development at the Royal Orthopaedic Hospital and Professor of Clinical Orthopaedics at Aston University, as well as Mr Jonathan Stevenson, Orthopaedic Oncology and Arthroplasty Consultant. The project is also supported by collaborators Professor Richard Martin and Dr Eirini Theodosiou from Aston University and Professor Joao Lopes from the Brazilian Aeronautics Institute of Technology.
Please note: This treatment is currently in the research phase, and is not currently in use at the ROH.