
Adult Acquired Flat Foot (Posterior Tibial Tendon Dysfunction)
What is Adult acquired flat foot / Flatfoot or Posterior Tibial Tendon Dysfunction (PTTD)?
This condition (which is know by various names) is caused by a dysfunction of the tendon (posterior tibial tendon), which helps to support the arch of the foot. For various reasons the tendon can become strained, inflamed, overstretched or torn resulting in pain and leading to flatfoot. The condition is progressive and should be treated as early as possible.
What are the symptoms of adult acquired flat foot?
The symptoms of this condition are varied and progressive in nature. These may include:
- Pain and swelling along the inside of the ankle
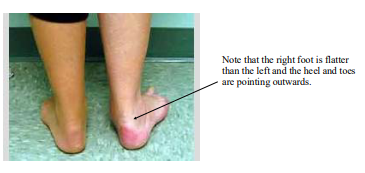
- Increased flattening of the affected foot
- Inability to raise up on to tip toe
- Pain which develops on the outside of the ankle
What are the causes of adult acquired flat foot?
These are varied and can include:
- Overuse of the tendon, due to poor foot mechanics (flatter foot) or overuse due to sports may cause damage to the tendon.
- Obesity - increased weight places additional strain on the tendon causing it to over-works, trying to maintain the arch height. It can then becomes inflamed, swollen and painful.
- Age related changes in the tendon - With age, the tendons lose their elasticity and ability to glide as smoothly as they used to. Thus, older individuals are more prone to developing symptoms of tendonitis, due to the impaired gliding motion of the tendon. When the tendon no longer functions properly, it becomes swollen, inflamed and painful.
- Previous injury, such as a ankle sprain, can tear the posterior tibial tendon or cause it to become inflamed.
- Systemic conditions - such as rheumatoid arthritis can effect the condition of the tendon
Additional risk factors for this condition include diabetes, and hypertension.
How is the condition treated?
Non surgical
Because of the progressive nature of PTTD, early treatment is advised. If treated early enough, symptoms may resolve without the need for surgery and progression of the condition may be prevented. In many cases of PTTD, treatment can begin with non-surgical approaches that may include:
- Orthotic devices or bracing to improve mechanical function and rest the tendon.
- Immobilisation - Sometimes a boot/cast is worn to rest the tendon. This is normally a short term measure. Wearing the boot for too long can lead to weakening of the tendon.
- Physiotherapy - Specific exercises to strengthen the tendon are extremely important for treating this condition. If done properly, it may prevent the need for surgery.
- Weight loss & healthy lifestyle - Being overweight will put additional stresses thorough the tendon. This can lead to tears and rupture. A healthy lifestyle including a good diet can be helpful.
- Pain medication - may be advised in some cases.
- Injection therapy - Injections may help reduce some of the pain, but can have side effects (e.g. tendon rupture) and isn’t a cure in itself. Physiotherapy is normally needed in conjunction with this intervention to strengthen the tendon. A boot is worn for approximately 1 week to protect the tendon following an injection.
Surgery
Surgery by an Orthopaedic Consultant may be indicated if non operative measure fail or in cases where walking is very problematic and painful. Surgery for this condition can be quite extensive and will often require a period in a cast of around 3 months.