
Flat Foot Correction in Young People
What do we mean by Flat Foot?
A flat foot is caused when the heel bone (calcaneum) tilts outwards away from the midline of the leg (valgus). This causes the instep (medial arch) of the foot to drop and forces the front of the foot upwards and towards the outside (see figure 1).
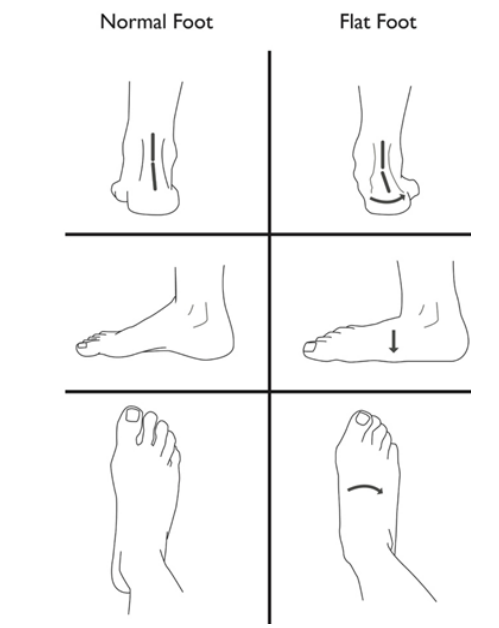
Figure 1
Do we always need to operate?
Flat feet are very common in young people and the vast majority do not have any symptoms or problems from them. If symptoms do occur, then usually they can be settled with insoles and heel cord (Achilles tendon) stretching exercises. Only those who do not improve with these methods are considered for an operation.
What do we do during the operation?
In order to correct the foot position, we first have to realign the heel bone and push its rear end towards the midline of the leg. This is done by cutting the bone near its front surface and inserting a wedge of bone taken from the top of the pelvis (the hard crest of bone near to where a belt sits). Sometimes this is held in place by a metal plate and some screws, but usually only a temporary pin is required (Step 1).
We are then able to judge how the shape of the foot has improved after this step. If further correction of the heel position is required, a second cut is made in the heel bone near its rear end which allows us to shift this piece of bone across. This requires a single screw to hold it in place (Step 2).
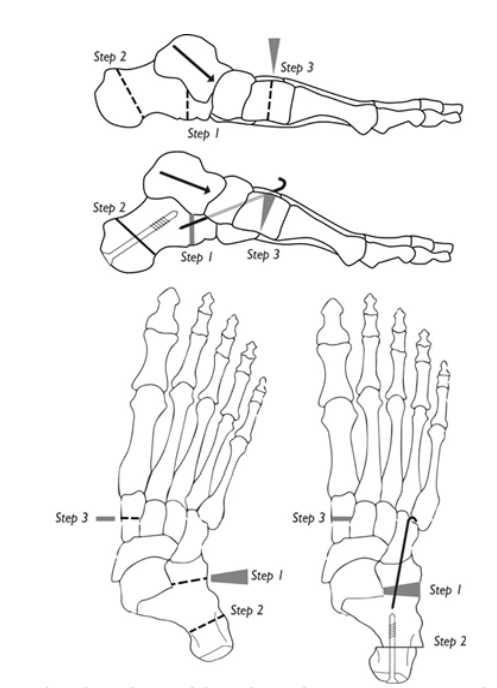
Once the heel position has been corrected, the front of the foot needs to be realigned as well to help recreate the normal arch. A cut is made in the bone from the top of the foot (medial cuneiform), just in front of the arch. A second wedge of bone taken from the pelvis is inserted, which brings the front of the foot down so that the big toe touches the floor deepening the arch (Step 3).
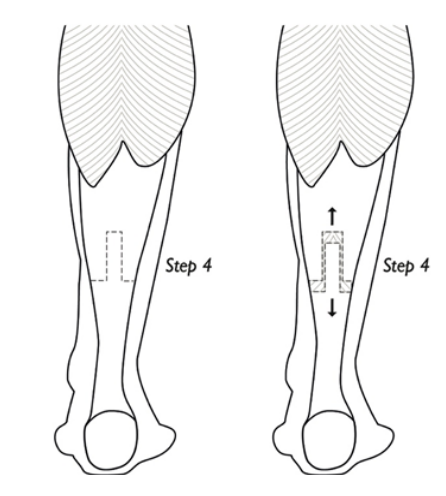
If your calf is tight which is very common with flat feet, we will also make a cut over the midsection of the calf muscle to release it and allow the ankle to move up more freely (Step 4).
Once the foot shape is corrected, the wounds are closed using dissolvable stitches. Dressings and a temporary, below-knee plaster splint or well-padded cast is then applied. Before you go home, the plaster splint if applied will be changed for a solid, longer-term cast.
How long does it take to recover?
For the first 6 weeks the cast will remain on and it is important that you do not put weight on the foot. This gives the bones that have been cut a chance to heal. For the first 3 weeks, it is important to keep the foot elevated as much as possible to reduce swelling and allow the skin to heal.
You will be seen in clinic to review the wounds at about 3 weeks and reapply the below-knee cast. Six weeks after the operation we will see you in clinic to remove the cast and the temporary pin. A plastic boot is then put back on for a further 6 weeks and we allow you to gradually increase the amount of weight you are putting on the foot until you are fully weight bearing at the pace that you can tolerate.
At the end of the 12 week period after the operation, the plastic boot will be removed and an x-ray will be taken. By this stage the bone is usually solid enough that you can get back into comfortable shoes, such as trainers. It will still ache at this stage but this will slowly settle over the next 6-12 month period and we will refer you for physiotherapy to strengthen the calf muscle.
If we are concerned that the bone is not healing as expected, then further x-rays or a CT scan may be required to assess the bone further.
Will my foot be normal after the operation?
Although your foot will be closer to the shape that we call “normal”, you will always notice that your foot looks a little different. Most people that have the operation still notice occasional aches and pains from the foot with strenuous activities, but these are usually mild and easily manageable with simple painkillers.
What are the risks?
Although we try to account for every eventuality, problems occasionally occur that affect the outcome of the operation. The majority of people that have the operation (85-90%) are happy with their feet after surgery. Those that are not happy usually feel that they did not get as much improvement as they would like, and a few have significant complications that leave them worse off than before the surgery.
Infection
This may affect 1-2% of people following surgery. It can range from superficial skin infections that require antibiotics to more severe, deep infections that need further surgery to clear up.
Nerve Injury
Any nerve near the area we are operating could be damaged during the surgery. This can result in numbness in parts of the foot or in nerve pain as the nerve tries to heal. Very occasionally further surgery is needed to treat the painful nerve.
Blood vessel injury
Blood vessels at the operated site can also be injured. These are usually small vessels that can be dealt with at the time of surgery. Occasionally there may be some bleeding after the operation that needs to be controlled by further surgery.
Joint stiffness
The joints around the bones that are cut will often become stiffer after the operation. Physiotherapy can help to improve mobility, but it may still feel stiff at times.
Bone and wound healing problems
The blood supply to the foot is not as good as other areas of the body as it is further from the heart. This means that sometimes things take longer to heal. It is important to keep the foot rested and elevated until the wounds have healed as this will reduce the swelling and tension. Keeping the weight off the foot for 6 weeks will also help the bones to heal. Smoking, diabetes and certain medications can also slow the healing process. Very occasionally the bones do not heal at all and remain painful. If this occurs then further surgery is likely to be required.
Problems with the metal screws/plates
Any metalwork that we use to stabilise the bones while they heal that is covered by the skin is designed to stay in for the rest of your life, unless a lot more growth is expected in the heel bone. Sometimes, the metal can be prominent and rub on the skin or a screw can loosen and back out. This occurs and causes pain in about 15% of patients and another operation to remove the metalwork may be required.
Hypersensitive scars
As the wounds heal, the surrounding skin will often feel numb. As the sensation returns, the area may become overly sensitive and may feel like pins and needles when touched. This can be helped by desensitisation methods and usually settles slowly over several months.
Pain
Residual aching is very common, but can usually be controlled by simple painkillers. More severe pain and pain syndromes are rare and can be quite debilitating and slow to recover.
Residual deformity
As previously mentioned, your foot shape will not be ‘normal’ after the surgery. Sometimes this is because we have not achieved as much correction of the foot shape as we would have liked to during the surgery or because we have corrected it too much. Occasionally, further operations are required to improve the shape. A very severe flatfoot deformity is more likely to remain slightly flat even after surgery. Fractures: Other bones in the foot breaking during the surgery is rare and the damage needs to be fixed at that time. Sometimes the bones we have operated on can break again before they have fully healed. If this happens then you may require a further period in a cast, or may even require further surgery to re-fix the bones.
Little or No improvement
Sometimes, despite correcting the shape, your foot remains problematic to the same degree as before the surgery. This may be due to a complication or may be due to other factors that we have not identified. Sometimes we cannot find a cause for ongoing symptoms, which often makes them very difficult to treat.
Worse symptoms
If complications occur, then a small number of patients (1-2%) feel that their foot is worse than before the operation was performed.
Blood clots
Being inactive in a cast increases the risk of forming a blood clot in the veins in your leg (a Deep Vein Thrombosis, or DVT for short). If you are over the age of 16, you will receive injections of blood thinners into your stomach for the first 6 weeks after the operation to try and decrease the risk of these forming. Despite this, clots can still occur and cause pain and swelling in the limb. Clots can also break off from the leg and move round the blood stream to the lung (a Pulmonary Embolus, or PE for short), although it is rare in young people. This can be life threatening, which is why we try hard to identify and prevent clots as much as possible.
Anaesthetic problems
General anaesthetic is usually very safe. However, the very rare complications that occur can be very serious and threaten your life. The anaesthetist will meet you on the day of surgery and give you more information about these risks.