
Tarsal Coalition
What is tarsal coalition?
A tarsal coalition is an unusual connection (sometimes referred to as a “bar”) between 2 or more bones in the feet. The connecting tissue can be either bone, cartilage or fibrous.
This condition normally occurs at the midfoot or hindfoot (under the ankle joint). Its thought that around 1% of the population may have this condition. The most common coalitions are:
- Talo-calcaneal (subtalar) coalition – a connection between the heel bone (Calcaneus) and the talus bone (which sits on top of the heel bone)
- Calcaneo-navicular coalition – a connection between the heel bone (calcaneus) and the bone in front of it (the navicular)
- Talo-navicular coalition – a connection between the talus bone and the navicular – this is quite rare.
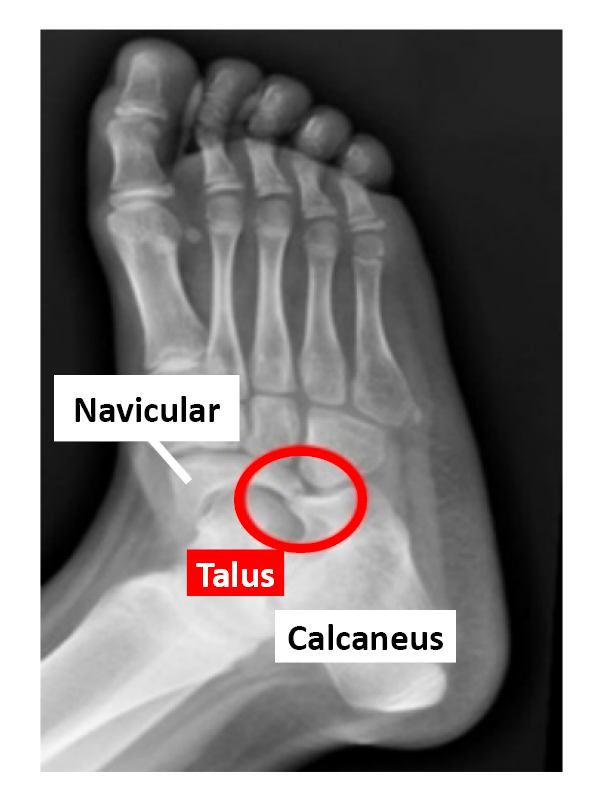
X-ray of a calcaneo-navicular coalition – showing the uncommon joining between the calcaneus (heel bone) and the Navicular bone (inside the circle)
What causes the condition?
It is thought to be due to an inherited and genetic abnormality, which results in the failure of some bones in the foot to properly separate in the embryo.
What are the symptoms?
Many people who have coalitions have no pain or other symptoms – they are asymptomatic. It is often not until late childhood, adolescence or even adulthood that symptoms develop. Pain usually occurs below the ankle around the middle or back half of the foot. Pain commonly starts when the bones stiffen (a process known as ossification). This usually occurs between the ages of 8-12 for talo-calcaneal coalitions and 12-15 for talo-navicular.
For adults, pain may be the result of trauma (e.g. an ankle sprain) or the development of arthritis in the joints. The tarsal coalition may be associated with a stiff flatfoot. Pain may come not only from the coalition itself, but from the peroneal tendons (which sit around the outside of the ankle). These tendons can shorten and go into spasm. Ligament strain and joint irritation may also generate pain.
Some people can present with frequent ankle sprains, foot stiffness and difficulty walking on uneven surfaces.
Many patients have both feet affected, though often the symptoms are only on one side.
How is the condition diagnosed?
The condition can be diagnosed through both a clinical examination (e.g. examining how the joints move) and with imaging (such as X-rays and MRI/CT scans). Findings in the clinical exam may include a flat foot with low arches, which is stiff (and doesn’t correct when you go up onto tip toe).
X-rays can help with the diagnosis, but often a high definition CT or MRI scan is required to give more detail, such as the size of the coalition, and to help with surgical planning.
What are the non-operative treatment options?
There are a number of non-operative treatments, which can be tried before considering surgery. These include:
- Activity modification e.g. Limiting high impact sports for a few weeks.
- Physiotherapy may help with stretching and strengthening muscles.
- Footwear changes, such as wearing an ankle boot (which limits joint movement) or using a rocker bottom shoe.
- Orthotic devices such as ankle braces or insoles may help some patients.
- Pain relief, such as non-steroidal anti-inflammatory medication may give some relief.
- Steroid injections (which acts as powerful anti-inflammatory) can reduce pain in some patients.
- A period of immobilisation for a few weeks can help settle the symptoms.
What are the operative options?
Surgery is normally considered when non-operative treatments fail and there is significant pain and functional limitation (e.g. you are struggling to walk or play sports).
Surgery normally involves either the removal of the coalition (known as a resection) or fusion (stiffening) of the joint(s). The choice of procedure(s) will depend on many factors and this will be discussed with your surgeon.
In general, a small surgical incision is made to give the surgeon access the foot joints. Key hole (“arthroscopic”) surgery may be possible depending on the size and location of the coalition. Talo-calcaneal coalitions are typically resected if they are less than half of the joint surface and if there is limited joint arthritis.
A graft (e.g. fat, or muscle) may be placed between the bones to stop it recurring. Re-alignment procedure(s) – for example a flat foot correction may be required alongside this resection procedure.
Calcaneo-navicular coalitions are generally removed surgically and a graft placed between the bones. After a resection (removal), younger patients will often make a full recovery.
A resection may not be viable if there is a large coalition and if arthritis present. In these cases, joint fusions (i.e. removing and stiffening the joint(s)) may be indicated. The aim here is to sacrifice painful movement for pain reduction.
It is important to note that surgery for this condition will not result in a “normal” foot. As the articulations (joints) were abnormal to begin with, the foot after surgery, will remain stiffer than a normal foot.
What are the risks?
As with any surgery there can be complications with surgery. Some of these complications will be specific to the type of operation you have (e.g. fusion, resection, flatfoot correction). Your general health, wellbeing and lifestyle can impact on the success of the operation.
General risks
- Infection (superficial, deep)
- Nerve damage
- Blood vessel damage
- Tendon injury
- Wound healing issues
- Hypersensitive scar
- Worse symptoms
- Increased pain
- Eecurrence (return of coalition)
- Blood clot (DVT/ PE)
- Anaesthetic risks
Specific risks for resection of the coalition:
- Incomplete resection (not taking away enough bone)
- Recurrence (c. 10%)
- Over-resection (taking too much bone away)
- Worsening flat foot and persistence pain.
- Ongoing symptoms are more likely with a talo-calcaneal resection and in older patients.
Specific risks for joint fusion:
- Delayed union
- Malunion (bones fuse in wrong poison)
- Non-union (bones don’t fuse together)
What is the post-operative recovery?
Recovery will depend on the type of surgery you have undergone and how well you heal. The information provided below is for resection surgery only. There are additional leaflets available for fusion operations.
When can I...
Walk after surgery
After a resection operation you will routinely be in a non-weightbearing cast for about 2 weeks. You should keep the foot elevated (foot above the knee) for about 95% of the time during this period. After 2 - 3 weeks the wound(s) are checked and you may be placed into a special walking boot. This is normally worn for about 4 weeks. Physiotherapy may be organised at this stage. Sometimes patients can mobilise more quickly depending on the type of surgery and wound healing. It is worth remembering that it can take a few months for things to settle completely. Swelling and low-level discomfort may continue for 6-12 months.
Drive
Normally after 6 weeks. You can drive an automatic car before this if you had your left foot operated on and things are progressing well.
Return to work
This will depend on a few things such as – what work you do, how you are healing and what type of surgery you had. Overall as a guide, this can vary from 3-4 weeks for a sedentary type job to about 8-12 weeks for more manual/ strenuous type job.
Can this be a day-case operation - returning home on the same day?
It is usual to stay one night after the operation to allow adequate pain control. However, if you are otherwise fit and there is someone who can collect you afterwards and stay with you overnight, the operation can be done as a day case. This means that you are admitted to hospital, operated on and discharged home on the same day. You may need to come back to plaster room the day after your operation to have your plaster changed.
Will I have to go to sleep (general anaesthetic)?
The operation is usually performed under general anaesthetic (asleep). Alternatively, an injection in the back can be done to make the foot and ankle numb while you remain awake. Your anaesthetist will advise about the best choice of anaesthetic for you.
Wellbeing advice
Patients that have a healthy diet and weight, take regular exercise and refrain from smoking prior to surgery are more likely to experience quicker and better recovery and may also have a more successful outcome from their surgery. If you have any concerns about your general health and wellbeing (diet, exercise, smoking cessation) you are encouraged to discuss this with your GP, who will be able to provide advice on the options available to you.