High Tibial Osteotomy and Distal Femoral Osteotomy
What is an Osteotomy?
An “osteotomy” is a surgical procedure that aims to realign the bones of your knee in order to reduce the pain and symptoms you have in your joint.
Why do I need one?
An osteotomy is done for a number of reasons. It may be to correct a problem with developmental alignment of the bones that may cause you problems later in life if left untreated. In this case, an osteotomy aims to line the bone up correctly with your joint and restore a more normal alignment.
You may have a single hole in the surface of your joint cartilage, or more widespread degenerative changes (osteoarthritis) in one area of your knee joint.
An osteotomy may also be recommended to you in order to treat instability (wobbliness) and may be performed in combination with another procedure at the same time e.g. ligament reconstruction.
Normally, when we are walking or standing, the weight goes through the centre of our knee. Some people, however, are born with knock knees, causing the weight to be placed on the outside of the joint, or bowlegs causing the weight to be placed more on the inside of the joint. The process of injury or disease can alter the normal position or structures within the knee joint. For example, if wear and tear affects one side of the joint, it can cause a bow leg or a knock knee. The change in alignment can cause pain due to the increased mechanical stress. When this happens, more weight is taken by a specific part of the joint, which in turn, causes more wear and malalignment and becomes more painful and symptomatic over time.
This surgical technique can be an effective way of restoring a more normal alignment of the knee or in the case of arthritis, prolonging the life of your own knee, relieving pain and restoring your quality of life, sometimes for many years. It is often recommended for patients who are younger and more physically active. This group of patients are not recommended to have joint replacement surgery due to the high risk of the knee replacement loosening and early failure of the joint requiring a further revision knee replacement. If this applies to your case, your surgical team will have discussed this with you.
What is involved in the surgery?
The principle behind osteotomy is that by realigning your leg, your weight is redistributed off the damaged area of your knee and onto the healthy side of your knee joint. It involves cutting either the tibia (shin bone) or the femur (thigh bone) and sometimes in very severe cases, both bones. The alignment of the bone is carefully adjusted by either removing a wedge of bone or opening the cut (like a door hinge) to create a gap until the desired alignment is reached.
The new position is then secured with metal screws and a plate, which will hold the bones until they heal. The main aim of the surgery is to give you a more comfortable knee than the one you currently have.
You may be undergoing a high tibial osteotomy or a distal femoral osteotomy or both, depending on which part of your knee has suffered the problem. You may be having other procedures done as part of this surgery such as cartilage repair or ligament reconstruction. Your surgeon or other health care professional will advise you accordingly.
What are the advantages of an osteotomy?
The main advantage of an osteotomy is to help relieve the pain you currently feel in your knee. It corrects mal-alignment and as such, helps prolong the life of your knee joint, preserving it and delaying the need for further surgery. Many younger patients who undergo realignment surgery go on to maintain an active lifestyle for many years. Some even return to manual work or sport; ask your healthcare professional if this is likely to be the case for you. Approximately 75% of patients will not require any further surgery within 10 years following an osteotomy.
What happens during the operation?
You will be expected to stay in hospital for a night or two, depending on how quickly you recover. It is classed as a major operation and usually takes approximately 1-2 hours. The operation will be done under general anaesthetic, meaning you will be asleep for the duration of your surgery. You may also have spinal anaesthetic to help with the pain you might feel afterwards.
Often, your surgeon will do a keyhole operation at the time of surgery prior to doing your osteotomy to double check your suitability. If at the time of arthroscopy, it is found that you are not suitable for the osteotomy, then the procedure will finish and you will potentially be able to go home the same day. You will have had a special X-ray prior to your operation which allows your surgeon to plan your procedure accurately and during the procedure X-ray screening imaging will also be used. During the osteotomy operation, your surgeon will make accurate surgical cuts in either the tibia (shin bone) or femur (thigh bone) to achieve the planned correction of your leg alignment. The corrected bone is held firmly in place with a metal plate and screws.
Are there any alternatives to this surgery?
This varies depending on the reason an osteotomy has been recommended to you in the first place. Alternatives to surgery include managing your symptoms through pain medicines, changing your activity levels by perhaps avoiding physical activities that make your knee pain worse or changing your job. You may try steroid injections into the knee to help with pain. Sometimes, physiotherapy can be an effective way of helping your knee pain by keeping the muscles around your knee fit and healthy. A knee brace designed to off-load the part of your knee which is causing you pain can help. Generally speaking, most patients have exhausted these options hence this form of surgery has been discussed with you.
Are there any risks involved?
All operations involve a certain element of risk. Only you can decide how bad your knee pain and function is and whether it impacts of your daily life enough to commit yourself to surgery and the recovery it involves. The majority of patients who undergo an osteotomy make a good recovery and experience no serious complications, however, it is a major surgical procedure and it is important you understand sometimes problems can occur.
Medical/Anaesthetic risks:
It is difficult to separate the risks of anaesthesia from the risks of the operation and your general health. The risks to you depend on whether you have any other any other illnesses such as heart problems or diabetes. If you are a smoker or you are overweight the risks to you are significantly higher and, in some cases, surgery can be cancelled. Modern general anaesthetic is very safe however there are some common side effects. These include:
• Sore throat
• Feeling sick
• Shivering
• Headache
• Damage to teeth, lips or eyes
• Muscle Pain
• Excessive drowsiness
Serious complications to general anaesthesia are rare particularly if you are usually fit and well. Rare complications include life threatening allergy to drugs, breathing difficulties and cardiac issues such as heart attacks or stroke.
Infection – Superficial or Deep:
A deep infection most often starts when bacteria gain access to the tissues at the time of surgery. This operation is carried out in an ultra-clean air theatre and sterile clothing is worn by the surgical team. You will be given preventative antibiotics at the time of surgery. The risk to you is 1%.
You will not be discharged from the hospital unless the appearance of your wound is satisfactory. Once you are home, should you have any concerns about your wound please contact the ward you were discharged from. The risk of a superficial wound infection is 1%.
Damage to nerves and vessels:
The surgery is carried out next to a number of nerves and blood vessels. Injury to these nerves or vessels occurs in less than 1 in 100 patients. Any damage identified at the time of surgery will be addressed before the wound is closed. It is reasonably common to have some numbness over the outer aspect of your knee which usually decreases over time.
Swelling, bruising & numbness:
Due to the nature of the surgery, there will be some swelling of the leg, which will go down in about two weeks. There will be an area of numbness next to the scar which is entirely normal after surgery. Sometimes, initial bruising can be extensive, but should settle quickly. Ice packs and high elevation with your leg above the height of your pelvis can help. Do not elevate your leg on a low foot stool.
Blood Clots:
Blood clots in the leg (deep vein thrombosis) or blood clots on your lung (pulmonary embolism) are a risk associated with many forms of orthopaedic surgery. The risk to you is around 1%. The simplest way of reducing this risk is early mobilisation and although you may not be able to put weight through your operated leg, we will encourage you to mobilise with your crutches and to exercise your feet and ankles regularly. You will be given some compression stockings to wear to help minimize the risk to you. Please inform your surgical team or the pre-operative assessment team if you use any form of oral contraceptive pill or hormone replacement as this can increase your risk further. Drugs to thin your blood are not usually recommended as the risk of bleeding tends to outweigh the benefit of blood thinning drugs.
Delayed Healing/Non-Union:
In a small number of cases (4%), bone does not heal or takes longer than we would normally expect. You are at increased risk if you are a smoker, as this impacts the healing process significantly. If the bone fails to heal properly, you will require further surgery to your knee.
Potential Unexpected Fracturing of Bone:
Occasionally accidental breaks to the bone can happen at the time of surgery. Should this happen, the fracture will be addressed during your operation. This might slow down your
rehabilitation and you will always be told if this happens to you. Rarely, fractures only become apparent after the surgery. This would be monitored with repeated X-rays until the bone heals.
Loss of fixation or displacement:
Rarely, the fixation can fail or come loose, perhaps as a result of failure of the surgical implant e.g. a screw breaks. This will usually always require further surgery to rectify. The risk to you is less than 1%.
Bleeding (requiring transfusion):
Bleeding is rare, but some bruising may still occur. If a collection of blood results (haematoma), it may need to be drained. Rarely damage can occur to blood vessels behind the knee; this can lead to loss of circulation to the lower leg and foot, which may require further surgery. If you were to lose a lot of blood you may need a transfusion.
Stiffness:
Post-operative stiffness can occur as the knee responds to the trauma of the surgery. Sometimes, scar tissue builds up inside the knee, restricting your movement significantly. Here, you might need water based physiotherapy or a further surgical operation to address it.
Ongoing or Unresolved Pain:
Having an osteotomy does not rid your knee of any disease. For a small number of patients, despite off-loading the diseased part of the knee joint, they will continue to get some symptoms/pain as a result of the underlying arthritis. Around 85% of patients report good to excellent results once recovered.
Compartment Syndrome:
Compartment syndrome can occur as a result of increased pressure around the muscles of the lower leg as a consequence of bleeding or swelling. This requires extended hospital stay for monitoring and may mean further surgery on your lower leg to release the pressure. The risk to you is less than 1%.
Irritation from Metalwork:
Some patients can feel their metal plate just under the skin. In many cases, it can irritate the surrounding soft tissues and cause pain or discomfort. For these patients, it is usually recommended the metalwork is removed, but only after a year from surgery. This requires another operation with a 2-4 week recovery time. This is the most common complication from surgery.
What happens after surgery?
When you wake up, you will have a bandage and you may have a special brace around your knee, but only if you had other procedures performed at the same time as your osteotomy. You will have a wound that will require some nursing care at 2 weeks after surgery. You must keep this clean and dry until you are asked to see your practice nurse at your GP surgery. Your brace (if you have one) is designed to restrict movement at certain intervals and you will be asked to wear it at all times for the first 4 or 6 weeks. It should be adjusted at particular time scales in your recovery – your nurse, physiotherapist or doctor will explain this to you as applicable.
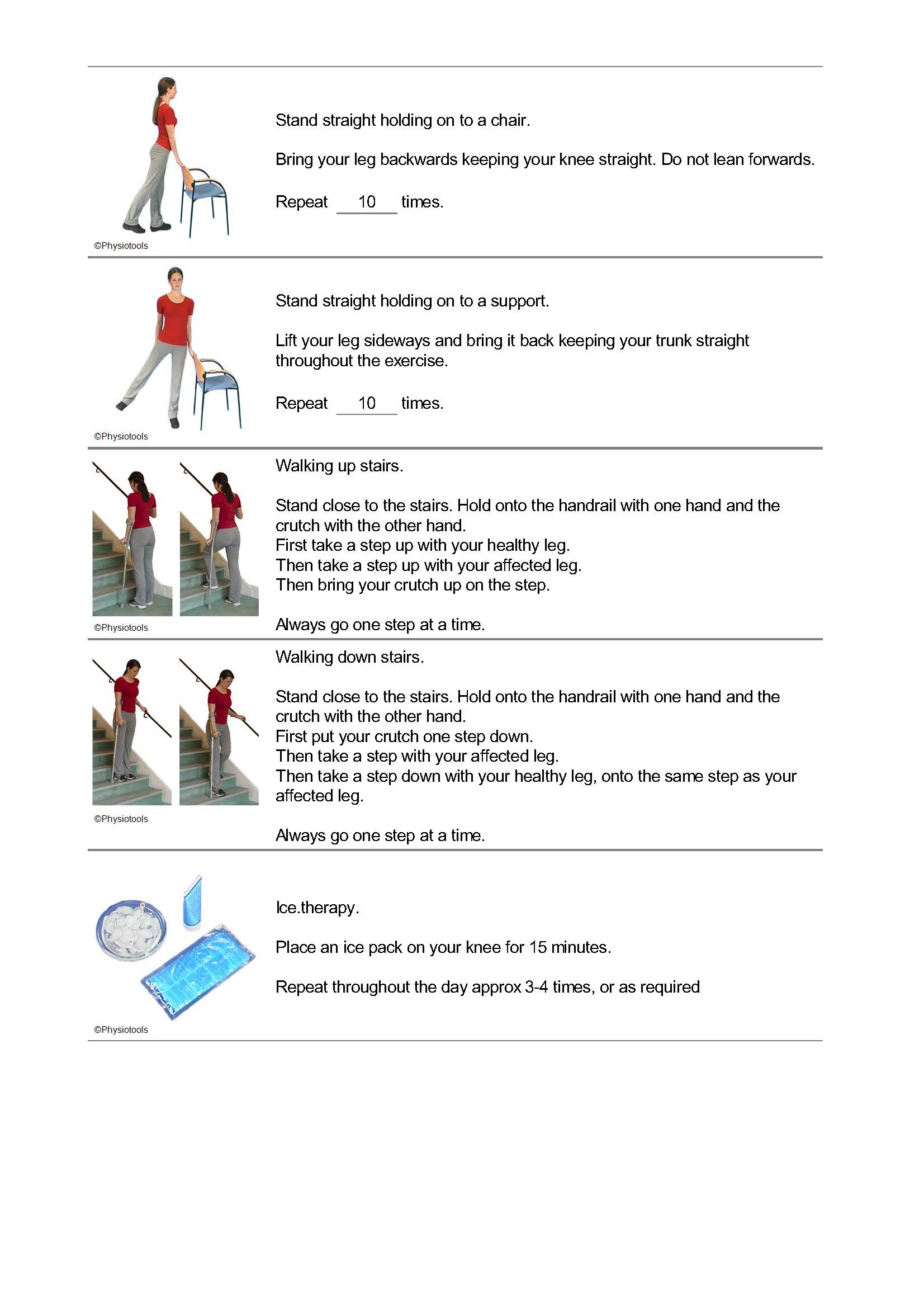
You will either be asked not to weight bear on your operated leg or to put partial weight through it when you walk. Both of these requirements mean you will need to use 2 crutches at all times. The physiotherapy team on the ward will talk to you about this. Sometimes you are allowed to weight bear again after 2 weeks. Sometimes we do not restrict you at all. This will be explained to you directly as each case is individual.
You should be prepared to take your recommended pain relief regularly and as advised by your medical team. The immediate few weeks after surgery can be difficult in terms of controlling your pain and swelling. You must also be prepared to work hard at the physiotherapy exercises given to you at the appropriate stages in your recovery. You will have some heat and swelling in the knee which is normal – be prepared to ice your knee regularly in the first 6 weeks of your recovery. You MUST elevate your leg above the height of your pelvis when you can. Regular icing will also help.
Typically, you will be able to go home the day after surgery. Your knee gradually heals over the course of about 6 months. You will be seen in outpatients a few weeks after your operation. You will need more x-rays at certain intervals in your recovery to ensure your bone is healing as we would expect. If you have not received an appointment, it is essential you phone the appointments office on 0121 812 3200.
Driving:
You must not drive for 6 weeks following your surgery. Doing so may render your insurance policy invalid. After this you may drive when you are comfortable and safe to do so. Ideally, you will have stopped using crutches and be able to sit comfortably. You should have enough power and bend in your knee to perform an emergency stop. You may get back to driving quicker if you have an automatic car. The law states you should be in complete control of your car at all times. It is your responsibility to ensure this.
Returning to work:
You are likely to be away from work for anywhere up to 3 months after surgery. This largely depends on what sort of job it is you do. Desk based workers can often return before, however you should remember that prolonged standing or sitting can make your knee swell and increase your pain. Patients with a more manual profession such as builders or other manual trades may not be fully operational for 4- 6 months. Your consultant’s team will advise you.
Sports & Exercise:
Your return to leisure activities will be guided by your physiotherapist and will depend on how you are progressing and whether you are reaching certain goals. Your therapist will advise you when you are physically capable to deal with different activities and will ensure you progress to a level where it is safe for you to return to certain activities. It is important to remember that you still have arthritis in the knee and there may always be some forms of sports and exercise you should not return to. Vary your workouts to include cycling, cross-trainer, rowing and swimming and other low impact cardiovascular exercise.
Physiotherapy:
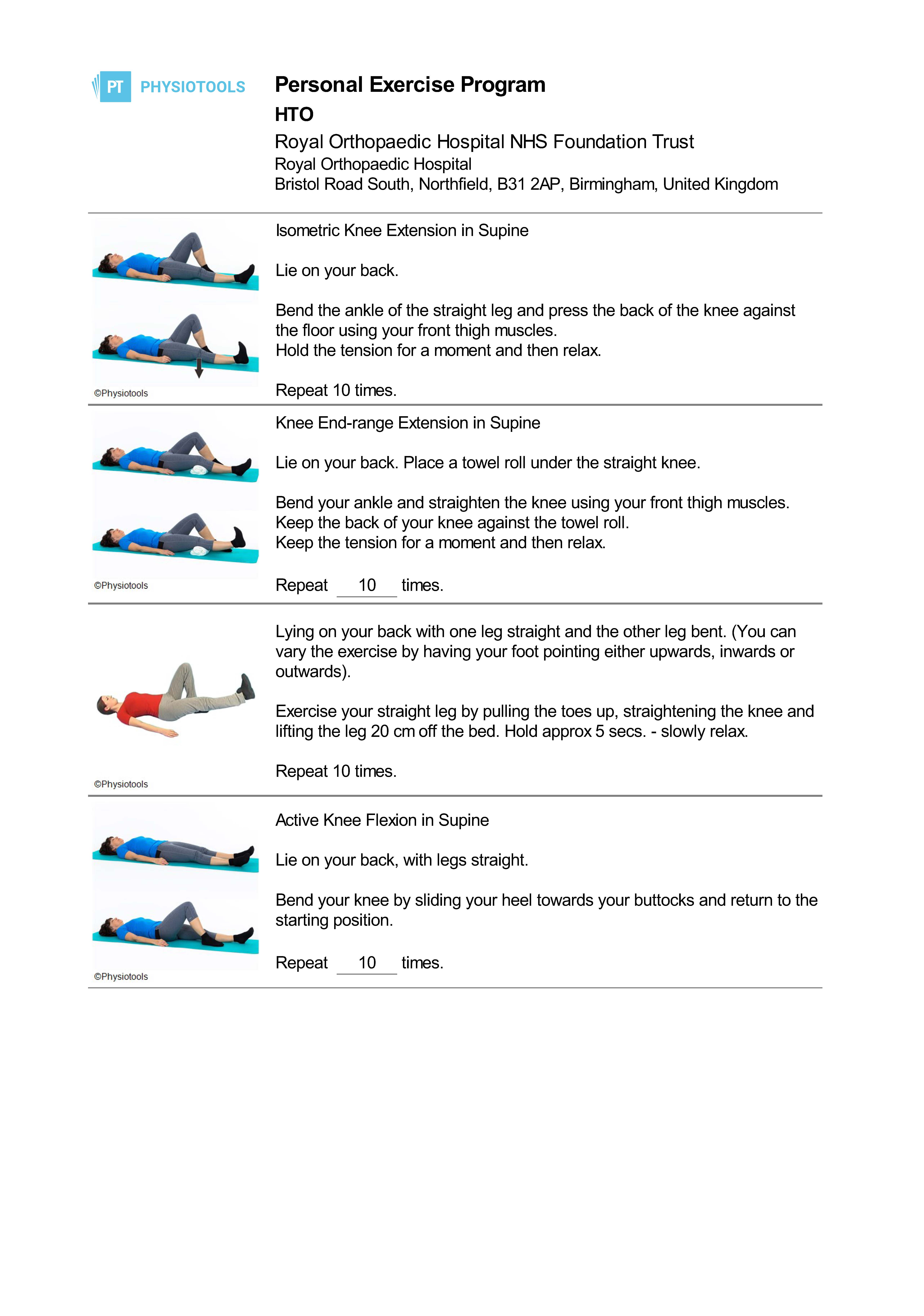
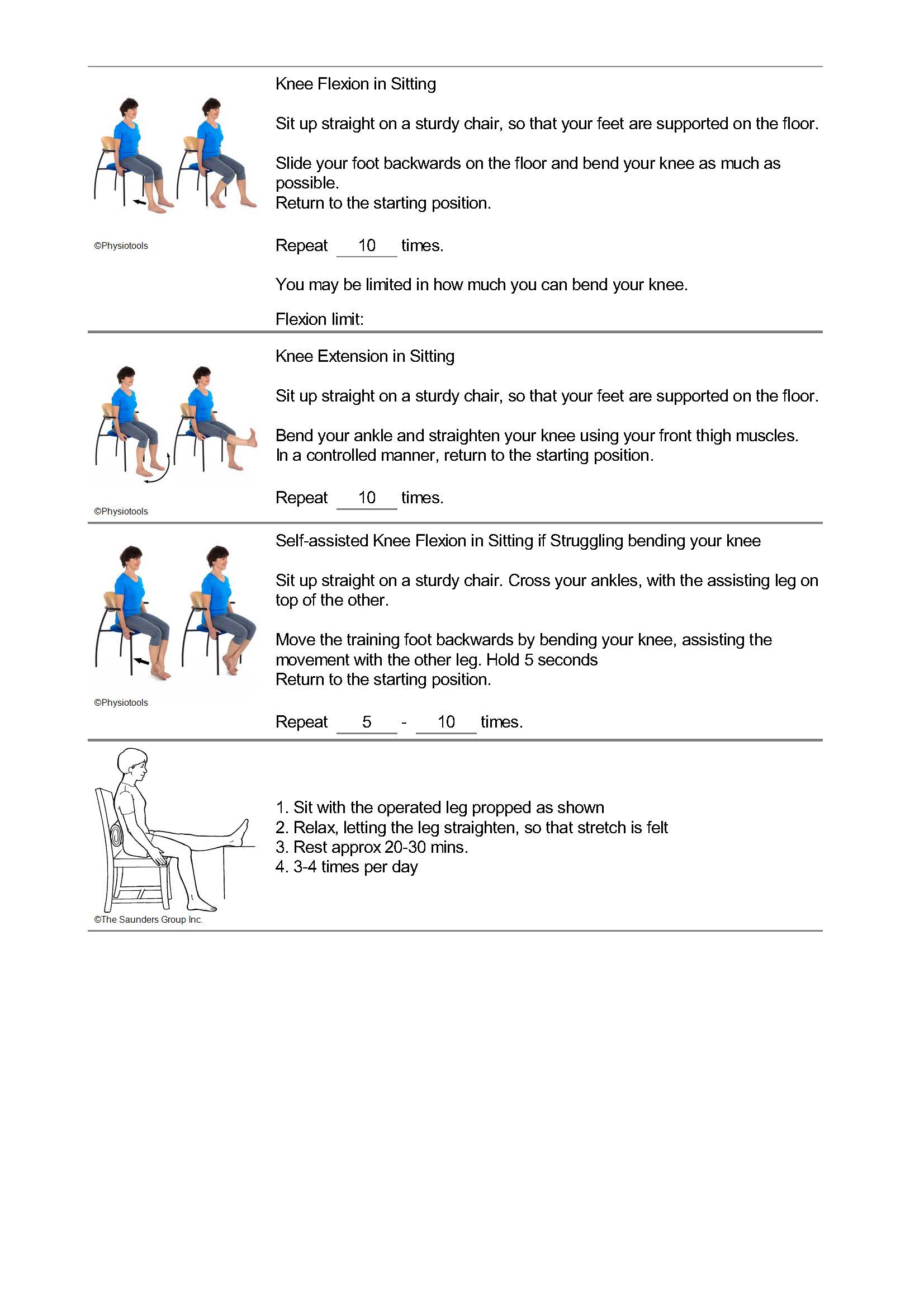
Your physiotherapy appointments should begin within two weeks of your operation and these will continue for several weeks until you are able to return to your normal pre-surgery activities. Whilst you are waiting to see your physio, you should maintain these exercises as often as your pain allows.