Anterior Shoulder Stabilisation
What is a shoulder stabilisation and why is it needed?
General looseness of the joints or upper limb injuries can cause your shoulder to become unstable. This tends to be more common in younger patients or those who participate in racket or overhead sports. You may have suffered previous dislocations which have required hospital treatment or be experiencing symptoms of pain and instability due to partial separation of the bones (subluxation) when your arm is held in certain positions. This can cause disruption to the delicate structures deep within the ball and socket joint (Glenohumeral Joint), including the joint lining (which is known as the labrum) and the surrounding ligaments.
The labrum can be separated from the bone at various points, or the capsule which also helps to keep your shoulder in the correct position, can weaken. Ligaments may become stretched or even torn. Sometimes the bone surfaces may be affected. You may have only one, or more commonly, a combination of problems with these structures. Your doctor/nurse will be happy to guide you through the anatomical problem that is specific to you. By surgically stabilising your shoulder, it is hoped that these symptoms will resolve and that you can return to your normal work/sports/hobbies.
What does it involve?
The operation is usually done via a keyhole (arthroscopic) procedure, although sometimes your surgeon may have to do an open operation if your shoulder has dislocated many times and there is damage to the bone surfaces, or the ligaments have been stretched too far. This will be discussed with you during your clinic visit before you come into hospital. Generally, stabilisation surgery is done as a day case procedure and provided you are well and have someone at home, you will be able to leave hospital the later the same day.
What are the risks?
- There is a small risk of infection
- There is a small risk relating to general anaesthetic
- There is a small risk that your shoulder may become unstable again
- Nerve injury can also occur for reasons outside the surgeon’s control
What happens in surgery?
You will be escorted to theatre by your allocated nurse and will be taken to the anaesthetic room. Here, the surgeon and anaesthetist will greet you. You will require a general anaesthetic. If you have questions regarding this you will have time to consult with your anaesthetist prior to your operation. A nerve block may be used before the operation which means immediately following surgery your arm and shoulder will feel numb. This helps with pain but will wear off after a few hours, so regular painkillers are advised and will be supplied by the hospital. Following your surgery your arm will also be supported in a sling with a body-belt attached. Arthroscopy allows your surgeon not only to look inside, but to treat your shoulder joint using a small TV camera. This has the advantage of smaller scars and less pain when compared to open operations. Once inside, the surgeon is able to repair the underlying problem using special suture material and tiny metal anchors, or by tightening the over-stretched soft tissues. Again, treatment will depend on the type of problem you have.
What to expect after surgery
Your shoulder may be sore for a period of up to 3 weeks afterwards. It is advised that you continue taking your painkillers as prescribed during this time. Use of ice packs may also help by reducing the amount of inflammation in your shoulder. Ice packs should be made from ice cubes in a plastic bag and wrapped in a damp tea-towel or pillowcase. Ice should never be directly applied to the skin as this can cause ice burns. Frozen peas or purpose made ice packs from the pharmacy are also ideal. The most effective duration of application of ice is 20-30 minutes every 2-3 hours. Ice should not be used if you have diabetes, Raynauld’s syndrome or in the presence of infection. Care should be taken if you have an existing heart condition. If you have, ice should not be applied to the left shoulder. You will have a dressing on your shoulder covering 3 or 4 keyhole wounds. Sutures are not always used and due to the amount of fluid passed through your shoulder during the operation, wounds may leak for 3 or 4 days. Wounds should be kept dry and your nurse will advise you regarding this.
What about my sling?
When you return to the ward your arm will be immobilised in a special sling. This also has a belt that fits around your waist. Normally, you will have to keep the sling on for a period of 3-6 weeks to allow the repair time to heal. It should only be removed to do gentle exercises as advised later in this leaflet. Following the 3-6 week period, it should be removed completely to prevent your shoulder from becoming too stiff. You should still be cautious at this stage and should avoid any heavy lifting or strenuous activities. Your doctor or nurse will advise you further before you go home.
When can I go back to work/sport?
After the first 3-6 weeks your shoulder will be a little stiff and you will need help with Physiotherapy to regain movement and strength. They may also concentrate on postural exercise and special physiotherapy that retrains your muscles (Proprioception). Depending on the type of work you do you may be able to go back after 6 to 8 weeks.
For people who have a heavy manual job, this may be nearer 3 or 4 months. We would encourage you back to work as soon as possible, but this should not be detrimental to your physiotherapy regime. Returning to leisure activities again depends on what it is you like to do. Swimming is good exercise and the water helps to support your shoulder. Front crawl is not advised until at least 3 months, however breaststroke can be done when your arm comes out of the sling and of course, as your pain allows. Golf can begin at 8 weeks although racket sports should be avoided until at least 3 months. Contact sports such as football/rugby should not be attempted until 4 months and you should be guided by your doctor or therapist. Generally, it will be 7 or 8 weeks before you can drive.
Remember - Your shoulder will take approximately 3 months to significantly improve, with improvement continuing for up to 12 months.
Do I need to come back to clinic?
Yes. Your surgeon will request an outpatient appointment for you. This is usually at around 6 weeks although sometimes sooner. When you come to clinic you will be seen by a member of your consultant’s team. This may include senior registrars, clinical fellows, postgraduate doctors or a nurse practitioner. Each will be happy to discuss with you any problems or further questions you have. Normally you will be seen again at 3 monthly intervals until you are better. Sometimes you may need to be seen more often than this. If this is the case your doctor/nurse will explain why.
Should you experience any problems before your first clinic appointment or for advice, please contact your GP or any of the numbers on the back of this leaflet. Please remember, your consultant's secretary cannot give medical advice although will be happy pass on a message to a member of the clinical team who will call you back. If you have a query regarding an appointment, please call the central appointments office on 0121 812 3200.
When will physiotherapy start?
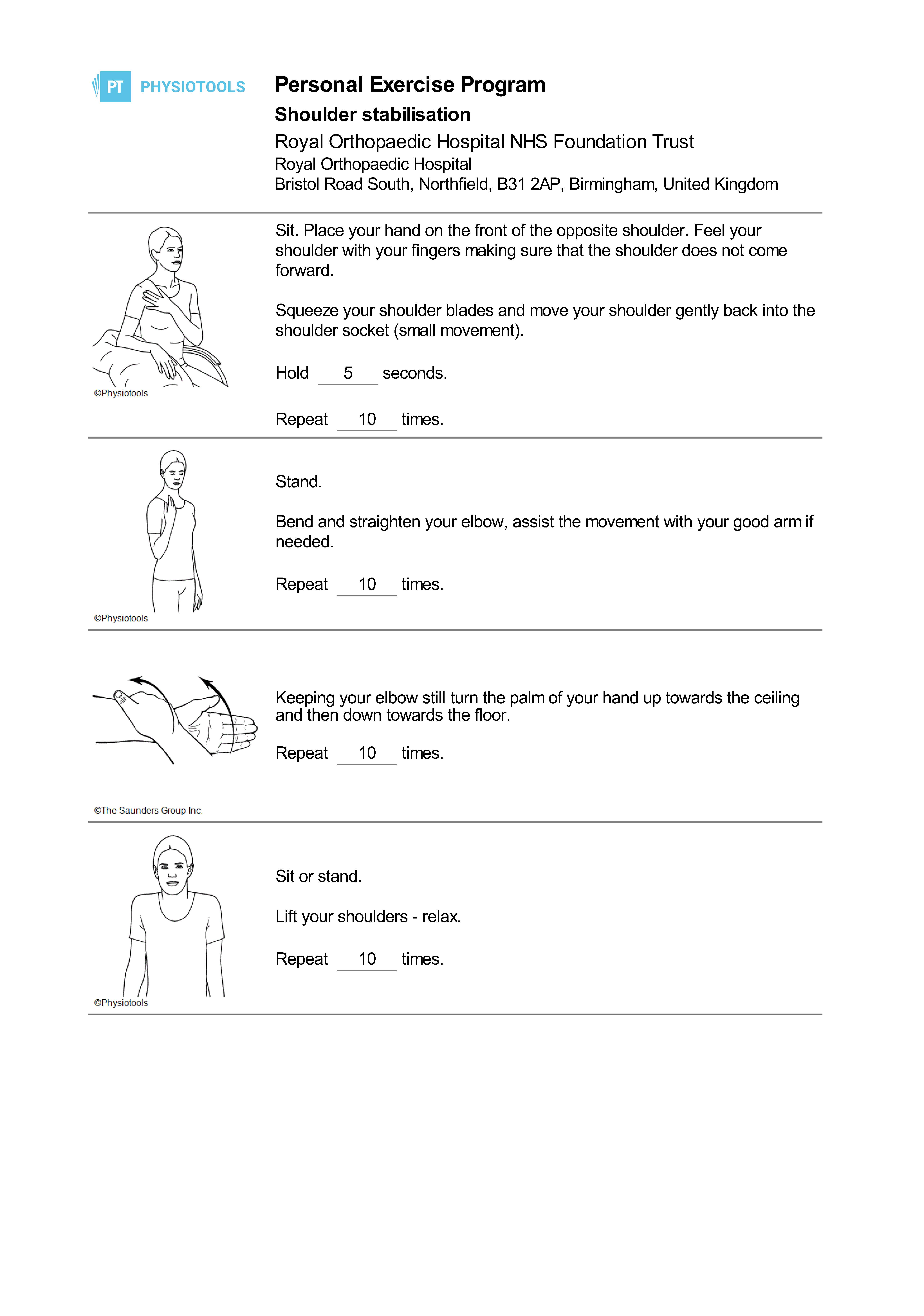
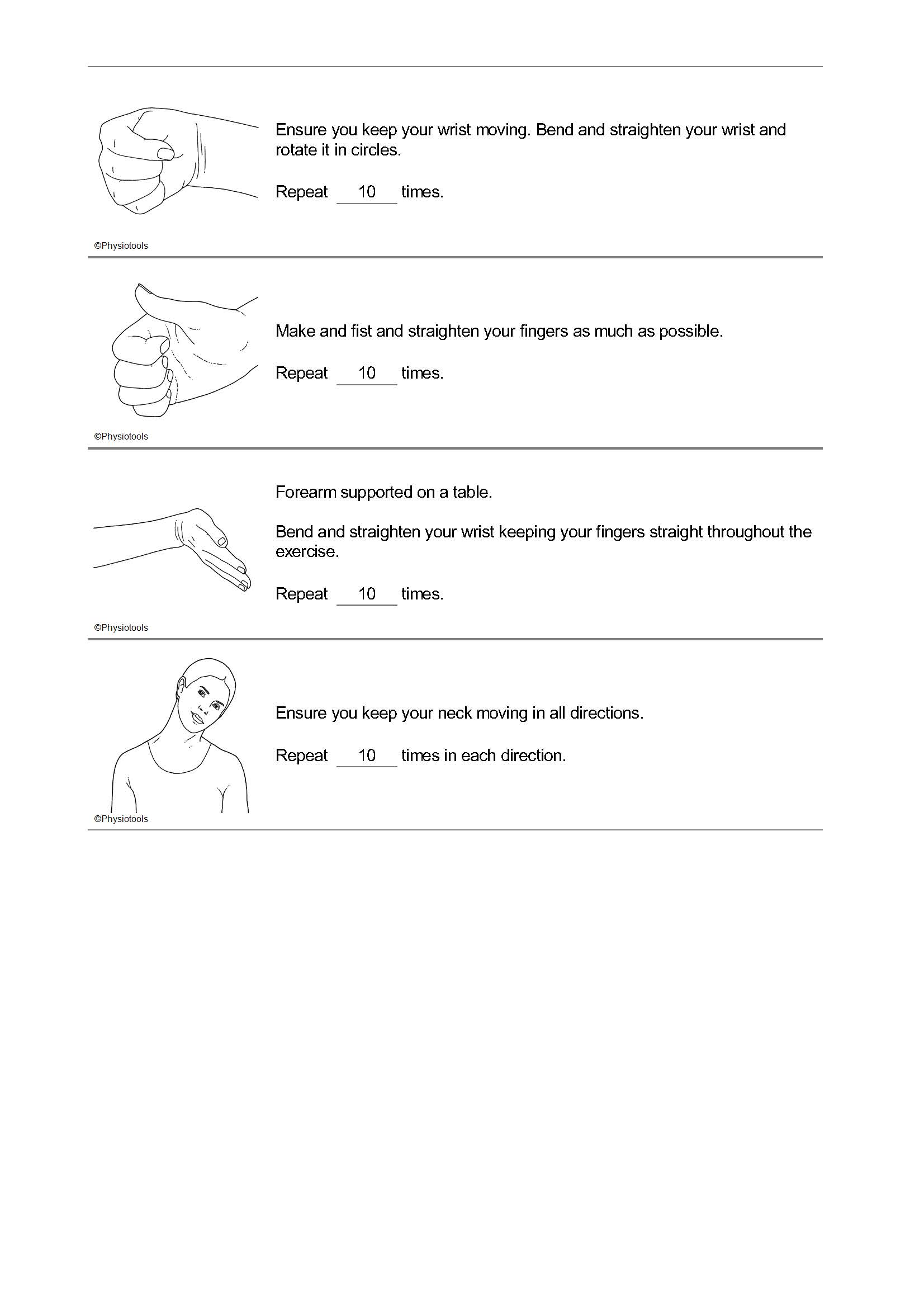
It is important that you do not use your shoulder for the first 6 weeks following your surgery. However, it is important to exercises regularly (3-4 times daily) following the exercises in this booklet so that other joints of your body do not get stiff.
You will require outpatient physiotherapy and this is usually done at the hospital nearest to where you live at about 6 weeks after your surgery. This will be arranged through the hospital and you will receive a letter at your home address asking you to call and make a suitable appointment.
Commitment to your physiotherapy regime is crucial in order to get the best outcome from surgery. Should you fail to receive any contact regarding physiotherapy, feel free to contact us and we can look into this on your behalf.
More information
If you have any questions or need any advice about your exercises, then please contact the Physiotherapy Department between 8am - 4pm Monday to Friday on 0121 812 3500.