Birmingham Hip Resurfacing
What is osteoarthritis of the hip?
Many factors may contribute to having arthritis; obesity, accidents, vigorous sport, or a family history may be important. In osteoarthritis (wear and tear), certain changes occur in the joint. Patients may need surgical intervention due to inflammatory, rheumatoid or osteoarthritis.
- The smooth cartilage becomes flaky and develops small cracks
- The bone underneath the cartilage becomes denser
- The lining of the joint becomes inflamed and may thicken up
As the arthritis progresses, there may be:
- Severe wear of the cartilage allowing the bones to rub and grate together
- Loss of the joint space
- Formation of bony lumps called osteophytes
These changes may result in pain, loss of movement and loss of muscle power.
Treatment options
Alternatives to surgery include managing pain through medication or injections or working with a physiotherapist to complete exercises or the use of walking aids.
About Birmingham Hip Resurfacing
The hip is a ball and socket joint. The BIRMINGHAM HIP Resurfacing (BHR) System is a conservative approach to replacing this joint, in which the moving surfaces (bearing surfaces) are made of metal. The BHR replaces the surface of the femoral head (ball) and acetabulum (socket), but preserves the bone within the rest of the femur including the neck . It was first implanted in July 1997 and was approved for use in the United States by the Food and Drug Administration in 2006. Since its introduction, there have been over 190,000 BHR implantations worldwide. BHR is the longest serving hip resurfacing device.
The Hip Resurfacing Procedure
The approach to the hip varies, but most surgeons tend to use a so called “posterior approach” (through the side of the hip and buttock area). Hip resurfacing procedures can cause a scar that may be slightly longer than a standard hip replacement as it is necessary to work around an intact femoral neck.
The acetabulum (cup) is prepared as for a hip replacement and a metal shell inserted with a friction fit. The worn surface of the head is then carefully reshaped, and a metal cap applied with cement.
After surgery, you will start walking with the help of two crutches for up to 6 weeks to allow soft tissue healing and getting used to your new hip. You will be discharged home after passing the physiotherapist assessment and when it is safe to go home. Your hip wound will be checked at approximately 2 weeks and if necessary, any stiches or clips removed. We tend to see you routinely in clinic at 6 weeks, unless there is any problem, in which case, you should call the ward which looked after you. You can also contact the consultant secretary if you cannot get through to the ward staff.
Benefits
The BHR is particularly suited active male patients requiring hip replacement. Hip resurfacing tends to be a better match to the size of the patient’s own hip. This reduces the risk of dislocation and some patients report the hip feels more ‘normal’. Resurfacing patients often report a quicker post-operative recovery in the short term and patients with a hip resurfacing are more likely to go back to sporting activities including competitive sports.
Features of the BHR include:
- Less bone resection than conventional total hip replacement
- Excellent, long-term clinical outcomes
- Less risk of dislocation compared to total hip replacement in active patients
BHR bone conserving system is well documented through independent clinical studies and national “joint registries”.
Suitability for Birmingham Hip Resurfacing
Birmingham Hip Resurfacing can only be used in male patients with a hip measuring greater than 50mm, this is because the complication rate including failure is higher amongst females and patients with smaller hips. Active males with osteoarthritis of the hip are most suitable for this treatment and seem to have the best results, with failure rates around 0.5-2% at 10 years.
Risks & Complications
General surgical risks:
Thromboses and emboli (blood clots)
Blood clots in the leg veins (deep vein thrombosis) and blood clots on the lungs (pulmonary embolus) are a risk associated with hip resurfacing surgery. The simplest way of reducing this risk is early mobilisation (exercises and walking). Whilst in hospital you will also be prescribed blood thinning treatment, usually in the form of injections, to reduce the risk of clot formation. Patients already receiving anti-coagulant therapy will be assessed and advised accordingly.
Urinary problems
Some patients, particularly those who may have previously experienced difficulty passing water, may sometimes need a catheter to be inserted into the bladder prior to or after the operation. There is a small risk of temporary incontinence; particularly in women, following surgery. Except in certain circumstances, this should be removed the morning after surgery.
Transfusion
Nowadays, blood transfusion following hip replacements is rarely needed. If your blood count is very low or if you are showing symptoms of anaemia (low blood count), the team looking after you may recommend a blood transfusion.
Fat embolism
This is rare and is caused by the fat within the bones (marrow) travelling up into your lungs at the time of surgery and causing breathing problems. Although this can be serious it is most commonly treated with extra oxygen therapy.
Superficial infection
You will not be discharged from hospital unless the appearance of the wound is satisfactory. Where possible, the dressing will stay on until the removal of your clips or stitches. After discharge, if you have any concerns about your wound, please call the ward.
Deep infection
A deep infection of the joint most often starts when bacteria gain access to the tissues at the time of surgery and great lengths are taken in theatre to reduce the risks of this happening. Operations are carried out in an ultra- clean air theatre and sterile clothing is worn by the surgical team. You will be given preventative antibiotics at the time of surgery. Despite all the precautions taken, infections can still occur. An early deep infection (within the first six weeks) may rarely occur, and this would require a further operation to clean the hip resurfacing. Occasionally it would be necessary to take out the hip resurfacing to resolve the infection. It is likely you would require a course of antibiotics.
An infection can occur at any stage in the life of a hip resurfacing. The reason for this is that any infection in the body can circulate in the blood and settle on the surface of the new hip joint. Once there it forms its own environment, or ‘bio-film’, which makes it difficult to treat with antibiotics alone. Although the symptoms of infection can often be suppressed with antibiotics the only way to eliminate this deep infection is to remove the artificial implant as described above.
Remember infection is a serious complication. If you develop any new redness around the wound or if the wound leaks after leaving hospital, it is important that you call the ward.
Bruising
It is common to see bruising around the hip in the days after surgery and, occasionally, this bruising will extend down the leg, sometimes into the foot.
Leg swelling
Leg swelling is a normal response to the operation and will settle week by week as your body absorbs the bruising. Exercises and walking can help reduce the swelling but standing unnecessarily should be avoided. If the swelling increases or if it is accompanied by tenderness in the calf or groin, a temperature or breathing problems you should ask your GP for advice.
Medical problems
Complications such as heart attack, stroke or death can occur after hip replacement as with other forms of major surgery. These complications are rare and the anaesthetist will not allow the operation to proceed if it is felt that the risks are significantly higher than normal. In this circumstance, it may be that you are sent for further tests or treatment prior to surgery being performed.
Specific risks:
Implant wear and loosening
On average, more than 90% of hip resurfacings in men are still working well after ten years. As with all artificial joints, wear and loosening can occur. If you experience new pain in your replaced hip, this can be a sign of loosening and you should seek advice from your GP or the orthopaedic team. Occasionally, loosening can occur without symptoms but may be seen on x-rays. It is for this reason that we will often follow you up with check x-rays for many years after your surgery, even though your hip may not be causing you any problems.
If your hip does loosen or become painful, your surgeon may recommend a revision procedure to a total hip replacement. This can be very complicated surgery and, should it be required, the risks and benefits of this would be discussed with you in detail.
Metallosis
The Birmingham Hip Resurfacing procedure has been tarnished by copy metal on metal resurfacing implants which through various design changes reduced the success of the procedure. As a result, the government issued guidance that means all patients with metal on metal implants are kept under long term surveillance (https://www.gov.uk/drug-device-alerts/all-metal-on-metal-mom-hip-replacements-updated-advice-for-follow-up-of-patients). Birmingham Hip Resurfacing has retained its original design and remains one of the hip resurfacing implants of choice with some of the best results. However, a small proportion of patients can develop so called “metallosis”. In metallosis small metal particles rub off from the implant and can lead to inflammation, allergy and damage to the local soft tissues and bone. This can cause ongoing pain and often steadily worsens. The treatment is to replace the metal bearing with an alternative implant typically a conventional hip replacement.
Dislocation
Dislocation occurs in a very small number of patients undergoing hip resurfacing. This may require a manipulation under anaesthetic to restore the alignment of the joint.
Fractures
Very rarely, fractures (breaks) of the bone can occur during the course of surgery. These are almost always identified during surgery or on the check x-ray after the surgery. Occasionally, this requires further surgery, or the surgeon may simply slow down your activities for several weeks to allow the fracture to heal.
Avascular necrosis
Sometimes the blood supply to the hip is damaged and the bone around the resurfacing then fails. This is rare but would usually require redo surgery to a conventional hip replacement if it occurred.
Leg length
The surgeon will try to ensure that your legs are of equal length but cannot guarantee this. Small differences may not cause any problems but if the difference is significant, it can be corrected by using a shoe insert or heel-raise on the appropriate side.
Nerve damage
Very occasionally one of the main nerves that run past the hip can be damaged during the operation. This can cause a foot-drop or paralysis of other muscle groups in the leg. Although the nerve often recovers over a period of months the paralysis can persist. The skin over the outer side of the hip can feel numb for up to 12 months until the nerve fibres recover - this is normal.
Aching in the joint, stiffness and or a limp
Most are delighted with their hip resurfacing. Some people describe aching or stiffness in the joint or have a limp which does not improve. This is rare and will be investigated thoroughly by the team looking after you.
Ectopic bone or heterotopic ossification (extra bone formation) The body may form new bone in the tissues around the hip in response to the trauma of the operation. This tends to occur only in the immediate recovery phase and may lead to long-term stiffness of the joint.
Tendinopathy
Some patients develop tendinopathy after surgery. This can manifest as pain either over the side of the hip or in the groin. The pain can often be helped with physiotherapy and exercises but in some cases can be persistent for months or even years.
What can I do to make the operation a success?
- Here are some things that you can do to help prepare yourself for your operation:
- Stop smoking: This reduces the risk of breathing problems and makes your anaesthetic safer.
- Have paracetamol and ibuprofen (if you are able to take it: supply at home for postoperative pain relief on your discharge from hospital.
- Speak to your dentist: If you have any loose teeth or crowns, treatment from your dentist may reduce the risks of damage to your teeth from equipment used during anaesthesia to support your breathing.
- Lose weight: If you are overweight, reducing your weight will reduce many of the risks of having anaesthetic and surgery.
- Speak to your GP: If you have a long-standing medical problem such as diabetes, asthma or bronchitis, thyroid problems, heart problems or high blood pressure (hypertension) you should ask your GP if you need a check-up and bring any results with you.
- Speak to us: If you are pregnant or breastfeeding so that we can make an appropriate plan for your surgery.
- Know your regular medicines: You will be advised what medication to continue and what to stop before you come into hospital. You must bring a complete, up to date list of your medication with you to all hospital appointments and on admission.
Preparing for your surgery
Fitness and diet
Do as much moderate exercise as your pain will allow, but in particular make sure that you do pre-surgery exercises you have been given.
Ensuring that you eat healthily in the days/weeks before your operation should help you to recover more quickly.
Stop smoking (including e-cigarettes) – your chest needs to be clear for your anaesthetic.
Drink alcohol only in moderation.
Healthy eating
If you are overweight and your consultant has recommended that you lose weight before your operation it is best to eat a varied healthy diet. This will help maintain your vitamin, mineral and protein levels which is ideal for an operation.
If you want more detailed information, please see the NHS Choices website or ask your GP to refer you to a community dietician.
General healthy eating advice
Eat more fruit, vegetables and cereals. Fruit, vegetables and cereals are all rich in vitamins and fibre (roughage). All fruits, vegetables and salads are beneficial and you should try and have 5 portions a day. Wholemeal/ wholegrain foods like wholemeal bread/pasta/rice, porridge, Weetabix and other high fibre cereals, beans, lentils and oats are also good for you
to try and keep healthy.
Cut down on sugar
Sugar contains no useful nutrients apart from energy and we can get all the energy we need from other foods. Reduce your intake of sweets and limit adding sugar to foods and drinks. Reduce sugar containing drinks.
On the morning of your admission
On the morning of your operation, have a bath, shower or full wash and wash and dry your hair. Do not apply deodorants, creams, products or make-up as you will be asked to remove it. Do not shave your operation site.
Please bring in your green medication bag containing all your medications. If you have a repeat prescription request slip normally attached to the green NHS prescription from your GP, please also bring this with you.
You will receive instructions on fasting and drinking prior to your admission.
What to expect when you arrive
- The anaesthetist and a member of the surgical team will visit you before surgery. The anaesthetist will explain the anaesthetic and methods of pain control. You will have the opportunity to ask any further questions. They will also discuss your consent again prior to surgery
- A member of the surgical team will draw an arrow on your leg to ensure the correct side is operated on. Do not wash off this arrow!
- You may be given pre-operative pain relief. This will help ensure that they are in your bloodstream before surgery
- You will be given an indication of the time you will be going to theatre. Theatres run all day so your surgery could be in the afternoon
- Before you go to theatre, you will be given a theatre gown to wear
- When it is time for your operation, one of our team will take you to the changing room. They will then go through a series of safety checks and then one of our theatre team will take over your care
- There will be a final series of checks before you are connected to monitoring equipment
- You will then be given an anaesthetic
What to expect - immediately after surgery
The operation to replace your hip takes approximately one hour.
At the end of the surgery, the anaesthetist will wake you up and take you to the recovery area. You may find several items in place to help your recovery. An oxygen mask over your mouth and nose helps your breathing. The drip in your arm should be removed once you are tolerating food and drinks. Your pain control will be established and your vital signs
monitored. Once you are fully awake you will then return to the ward.
Once back on the ward you will be given regular pain relief by the nursing staff in the form of an injection or tablet as required.
Observations including blood pressure, pulse, respiration rate, oxygen levels and temperature will be recorded. Your skin will be checked and our team will encourage you to change your position regularly to prevent pressure sores.
Pain management
You may experience some significant discomfort following surgery. You will be given regular painkillers, so you are able to do exercises and move your new hip. You should take the pain medication you have been prescribed whether you are in immediate pain or not.
Painkillers include paracetamol, ibuprofen-type drugs (non-steroidal anti-inflammatory drugs) and morphine-like drugs (opioids). Initially, you will need strong painkillers to help you to move. We will give you strong painkillers for one or two days after your surgery.
Please remember to let the doctors and nurses know if your pain is not controlled or above or if the pain stops you doing your exercises. We may need to alter or increase your painkillers.
Please don’t be afraid to ask if you need support managing your pain. We’re here to help you.
Some patients experience side effects. These can include:
- Drowsiness (feeling sleepy)
- Nausea or sickness
- Indigestion (heartburn)
- Constipation
If you have any concerns about your pain or the painkillers that you are given, you may discuss this with your nurse or doctor.
Back on the ward
- The consultant who operated on you will visit you to review your progress
- You will be encouraged to wash and dress
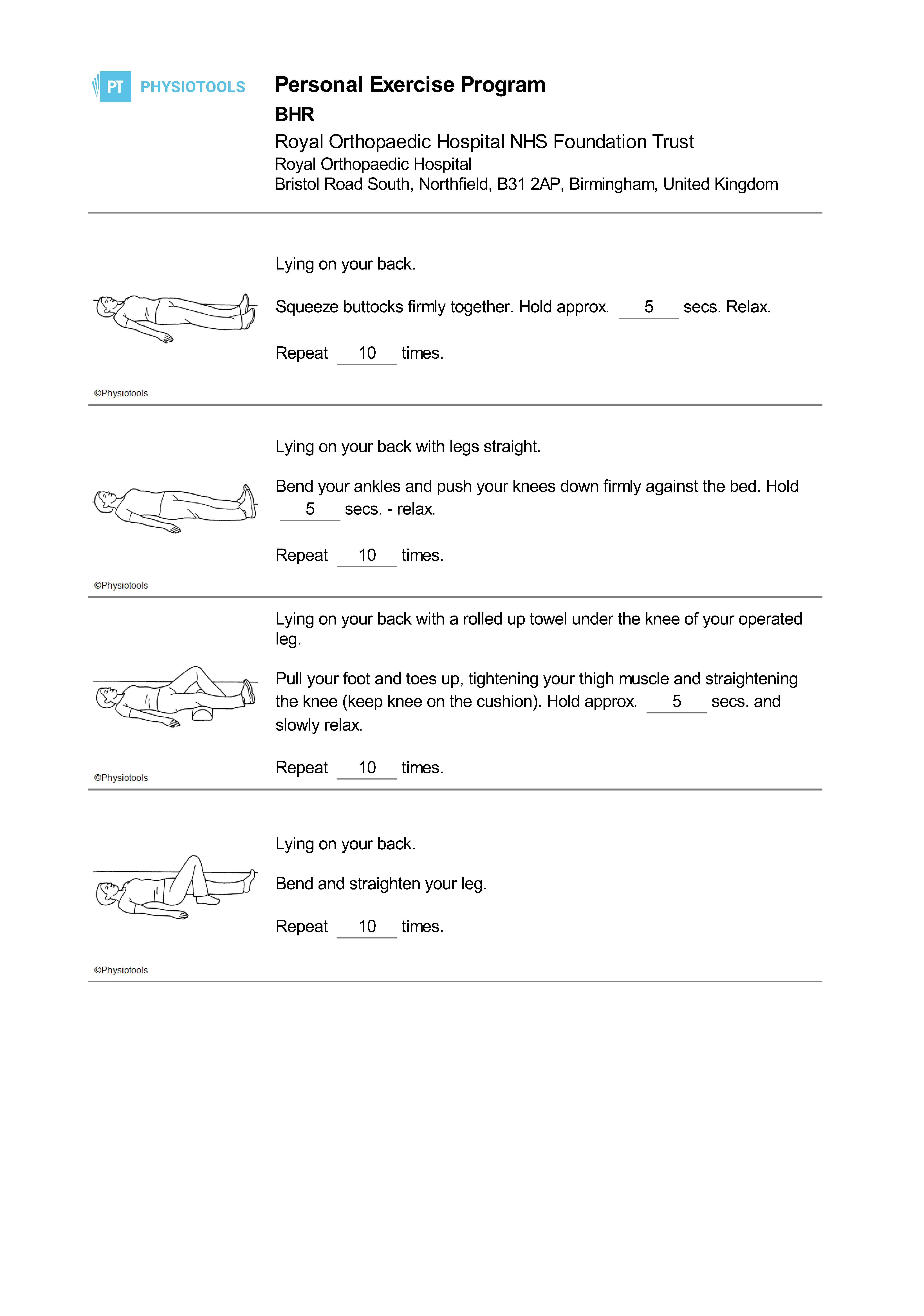
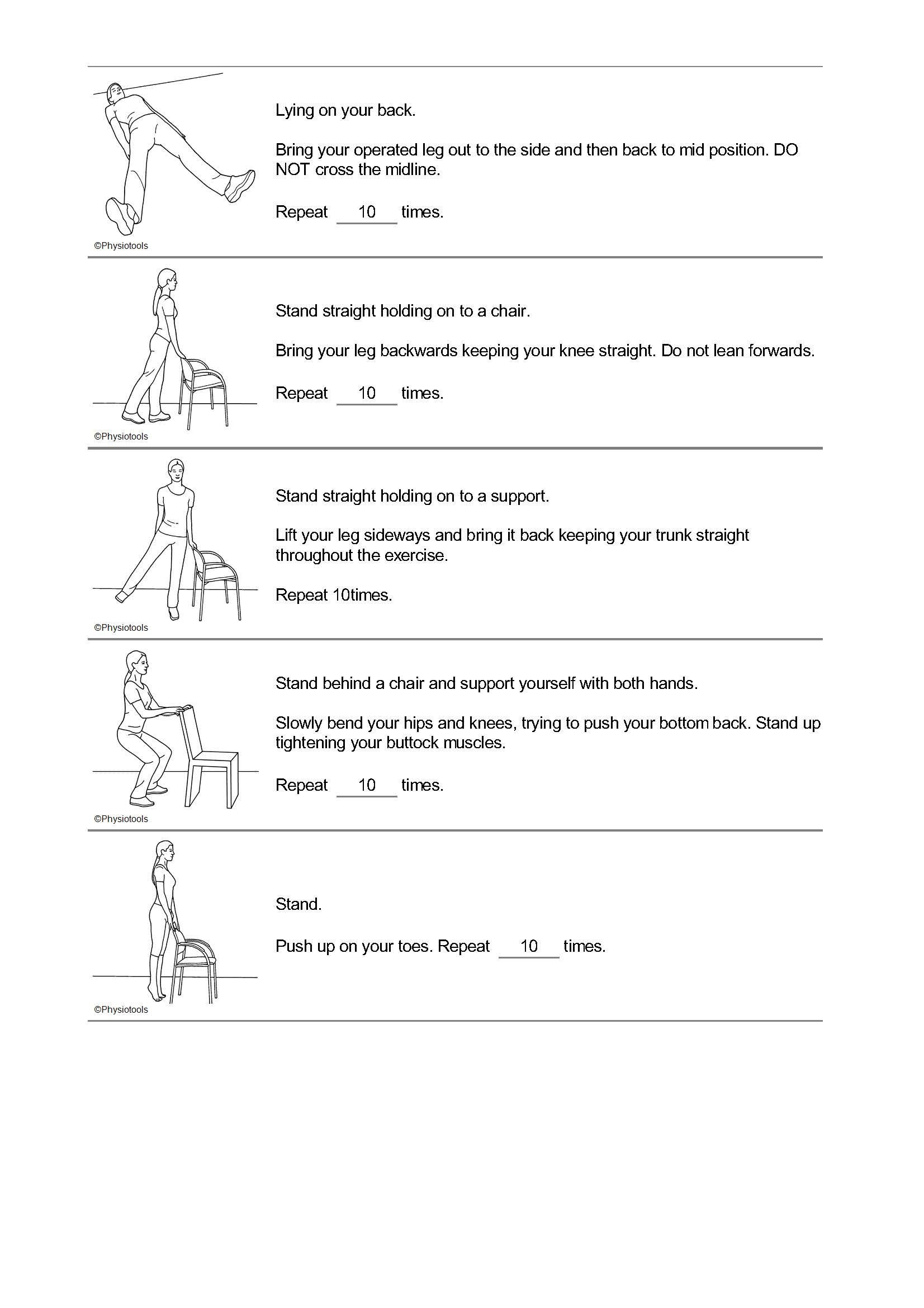
- The physiotherapist will see you and start your exercise regime
- You will be assessed and may be helped out of the bed to sit in a chair
- You will be encouraged to eat and drink
- The dressing on your wound will be checked
- Your pain levels will be assessed and pain relief will be given as appropriate
- It is possible the pain medication will make you constipated and so we will give you laxatives to help prevent this
- Throughout your stay, please let the nurses know if you have not had your bowels open so they can address the problem
Steps towards discharge
- You will be encouraged to sit in your chair for meals and encouraged to dress in loose fitting, comfortable clothing during the day
- The physiotherapist will continue with your exercises and progress your mobility with a walking frame or sticks/elbow crutches
- You will be encouraged to walk to the bathroom for your wash
- Blood tests will be taken
- You will have an x-ray of your new joint
- If you have them, your drain and catheter will be removed
- Please confirm your transport home with your family/friend
Back at home
You will be assessed prior to discharge to see if you require support from our community service – the ‘ROCS’ team. The team can visit you at home to offer further medical and physical support to aid your recovery. It is very important that you have organised the necessary support for when you return home. After major surgery you may feel that it is a good idea to ask friends or family members to stay with you or to help with simple chores. They will also be on hand to give you moral support.
General wellbeing
- It is not unusual to feel tired and your sleep patterns may take a while to return to normal. Remember to have your rest on the bed every afternoon for at least an hour to reduce swelling in your legs and feet
- Your appetite as well as your bowel habits may take a while to recover. Make sure you drink plenty of fluids and try to eat a healthy balanced diet
- Try not to feel frustrated at not being able to do all the things you want straight away. Increase your activity levels gradually. Start with short distances around the house and garden in the first 2 weeks then increase as you feel able
- Avoid tight clothing including belts and tight underwear. Loose garments are generally more comfortable and are a lot easier to put on
Eating
- Due to your reduced activity, you may lose your appetite or suffer from indigestion. Small meals taken regularly can help. If you have lost your appetite, then milky drinks provide a source of energy and goodness
Medication
- It is important that you continue to take all your medication as instructed
- You will have been given a supply of painkillers to take home. Continue to take these as directed until you no longer feel that you need them. Remember your pain should be controlled enough to allow you to move about comfortably and to be able to practice the exercises to strengthen your hip
- You may have been given tablets or injections to administer to thin your blood. It is important that you continue with these as directed
Compression Stockings
- If you have been told to wear your ‘Anti-Embolic’ stockings at home, apart from 30 minutes each day, these must be worn day and night for six weeks following your operation. The stockings should be hand-washed and dried away from direct heat to preserve their beneficial effect
Going to the toilet
- For the first two weeks after surgery it is very common for bowel movements to become irregular. This can be due to the effect of analgesia combined with inactivity and a change of routine. This will resolve itself as you get back into your usual routine at home
- However you can help yourself by eating high fibre foods such as fruit, vegetables and wholemeal bread. If necessary, try taking a mild laxative for a few days until you return to your normal routine. If you need any further advice regarding your diet please do not hesitate to ask
Washing
- You should follow the special advice given by the Occupational Therapy staff, which may include the use of special equipment, that will assist you to maintain your independence
- You may use a walk-in shower when you feel ready, but please do not have a bath for six weeks
Dressing
- When dressing, sit on the side of the bed or in a suitable chair. This will help your balance
- Collect all the clothes you intend to wear and put them on the bed next to you before you start. Avoid twisting and overstraining to reach them
- Always dress your operated leg first and undress it last
- Do not cross your legs when dressing e.g. putting socks on
Driving
Most patients are instructed not to drive for six weeks after their surgery, but your consultant will advise you on this.
For comfort, slide the seat back on its runners, recline the seat slightly to give yourself maximum legroom. It will be easier if the car is parked away from the kerb, so that you get into it on the level.
Make sure you can reach and use the pedals without discomfort. Have a trial run without the engine on. Try out all controls and go through the emergency stop procedure. Start with short journeys and when you do a long trip stop regularly to get out and stand up and stretch. Please be aware that if you drive soon after your surgery and have an accident, insurers may consider you liable for damage.
Sleeping
- You should try to sleep on your back for six weeks following surgery
- Changes in routine and restricted movement can cause difficulty in sleeping. Some people are awakened by the discomfort caused by sudden movement. If this happens, you may wish to take a painkiller to help you sleep
Continuing your activities at home
If you need to bend down to the oven, fridge, or low cupboard, you will find it easier on your new hip to take that leg behind you while bending the un-operated leg.
Safety and avoiding falls - all areas
- Pick up loose rugs, and tack down loose carpeting. Cover slippery surfaces with carpets that are firmly anchored to the floor or that have non-skid backs
- Be aware of all floor hazards such as pets, small objects or uneven surfaces
- Provide good lighting throughout
- Keep extension cords and telephone cords out of pathways. DO NOT run wires under rugs, this is a fire hazard
- DO NOT wear open-toe slippers or shoes without backs. They do not provide adequate support and can lead to slips and falls
- Sit in chairs with arms. It makes it easier to get up
- Rise slowly from either a sitting or lying position in order not to get light-headed
- DO NOT lift heavy objects for the first three months
- Stop and think. Use good judgement
Walking at home
If you are allowed to take full weight on your operated leg, you should use two sticks initially. When walking inside you may feel that you are able to use only one stick. You may do this when you feel safe and able to walk without a limp.
When walking with one stick remember to hold your stick in the opposite hand to the side of your operation. If you are not allowed to take all your weight on your operated leg, you will have been provided with appropriate walking aids by the physiotherapist and advised how to progress.
Sitting
Choose a chair that is comfortable for you but avoid low seats for the first six to eight weeks after surgery. Chair arms will help you get up and down safely in the first few weeks after surgery. To sit down and stand up safely, walk to your chair, slowly step back until you feel the back of your legs touching the seat. If you are using crutches, take your arms out of them and hold the handles in one hand.
Place your operated leg in front of you and place both hands onto the chair arms. Take your weight through your arms and un-operated leg, then ease yourself down onto the chair.
Once you are sitting, you can bend the knee of your operated leg, so your foot rests on the floor. Sit with your heels together, knees apart and toes turned out and don’t cross your legs.
To get up from the chair - reverse the process.
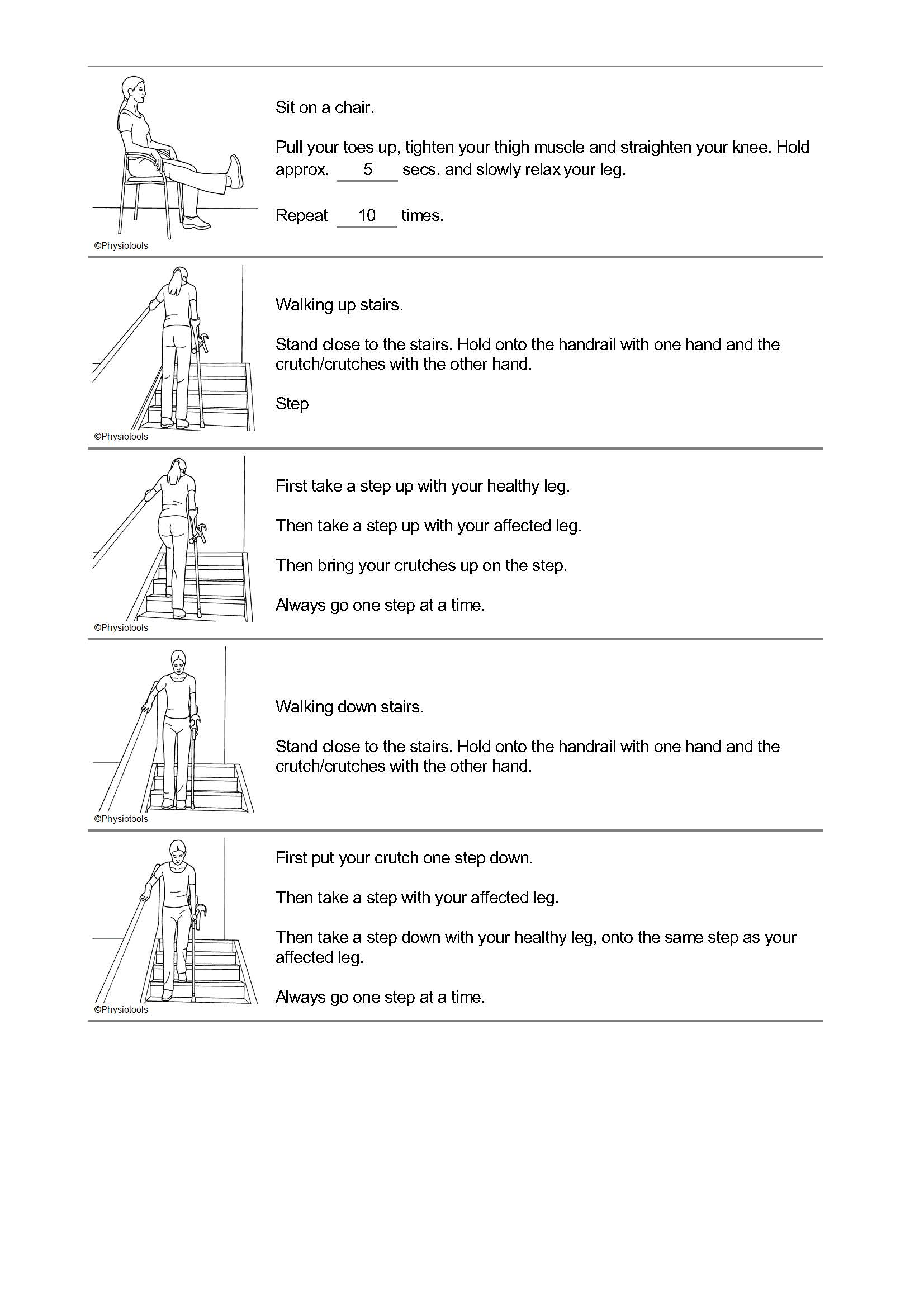
Stairs
Always use a handrail if there is one.
Going up - lead up with the unoperated leg, followed by the operated leg and the stick/crutch.
Going down - lead down with the stick/crutch and the operated leg, followed by the unoperated leg.
A lot of people use this to remember – “Up with the good, down with the bad”.
Keep this method up until you feel strong enough to walk upstairs normally. Many patients can manage this between weeks four and six (a few stairs at a time).
Household jobs
You should avoid all strenuous and taxing jobs immediately after surgery. Only when you feel up to it, should you attempt small chores and even then, ideally you should have somebody helping you.
- Do not get down on your knees to scrub floors. Use a mop and long handled brushes
- Plan ahead! Gather all your cooking supplies at one time. Then, sit to prepare your meal
- Place frequently used cooking supplies and utensils where they can be reached without too much bending or stretching
- To provide a better working height, use a high stool, or put cushions on your chair when preparing meals
- If you need to bend down to the oven, fridge, or low cupboard, you will find it easier on your new hip to take that leg behind you while bending the un-operated leg
Gardening
Avoid strenuous activity such as digging, pushing a wheelbarrow or mowing the lawn immediately after surgery. You may work at a bench in a greenhouse sitting on a high stool. Avoid reaching across your body for things. Avoid the temptation to do too much when you start gardening. Build up your strength, starting with lighter tasks and then progress as
your stamina increases.
Kneeling
Kneel onto operated leg first. Get up on un-operated leg first (let the un-operated leg take the strain).
Return to sport, leisure and work
- Low impact sports such as golf, bowls, cycling, swimming and walking may normally be resumed after three months. Check with your consultant at your follow up appointment
- High impact sports, i.e. jogging, singles tennis, squash, jumping activities, football are not recommended therefore are participated in at your own risk
- Return to work usually takes place between six and 12 weeks post-operatively
- Heavy manual work may require longer. Your consultant will guide you on this
Your physiotherapist can advise you about exercises and choice of sport.
Sexual activity
You are advised to refrain from sexual intercourse for six weeks after your operation and then resume with care mainly to prevent dislocation, muscle strain or injury around the hip. Choose positions that avoid twisting and excessively bending your hip. Our clinical staff are comfortable to give you advice. Please ask.
More information
If you have any questions or need any advice about your exercises, then please contact the Physiotherapy Department between 8am - 4pm, Monday to Friday on 0121 812 3500.
Further resources
https://orthoinfo.aaos.org/en/treatment/hip-resurfacing/