Hip Arthroscopy
Hip arthroscopy is a ‘keyhole’ procedure which allows a surgeon to visualise the hip joint and perform surgery.
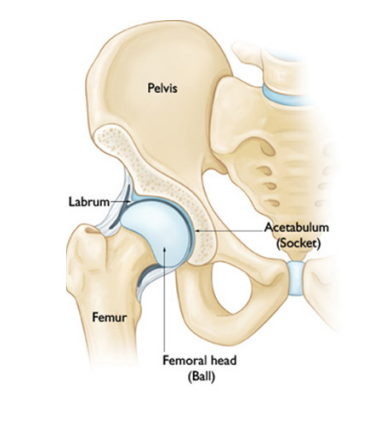
What does the hip joint look like?
The hip is a ball and socket joint. The ball of the thigh bone (femur) sits in the socket (acetabulum) of the hip. A ring of cartilage surrounds the socket and is called the labrum.
Why would a hip arthroscopy be needed?
Typically, the surgery is performed because of pain, clicking, “giving way and locking”, discomfort, stiffness or walking or running difficulty.
Hip arthroscopy surgery allows a surgeon to explore the joint and help find out the cause of your symptoms. The surgeon can remove or repair any loose or damaged tissue around the joint such as a damaged cartilage (gristle) or a torn labrum. Typically, the surgery is performed to treat one or more of the following problems:
- Femoroacetabular impingement Syndrome (FAIS)
- Acetabular labral tears
- Damaged ligaments around the hip
- Hip joint infection
- Swelling of the lining of the hip (synovitis)
- Investigation following hip replacement or hip resurfacing procedures
Effectiveness of hip arthroscopy
In general hip arthroscopy is about 70-80% successful at improving hip pain and improving quality of life for several years. However, some patients do not benefit at all and a small number approximately 5% are worse as result of this surgery. Worsening of symptoms is usually as a result of there being established and irreversible damage or arthritis within the joint, which surgery can sometimes exacerbate.
Am I suitable for hip arthroscopy?
The surgical team seeing you will help establish your suitability for hip arthroscopy. If you are markedly overweight the surgery may not be possible due to the limits of the instruments used for the procedure. As a rough guide if your Body Mass Index (BMI) is greater than 30 the team may advise you to try to lose weight before considering the surgery.
You can calculate your own BMI by using the NHS Calculator: www.nhs.uk/live-well/healthy-weight/bmi-calculator
What anaesthetic will I have?
Typically, a general anaesthetic is used and this is often supplemented with a regional local anaesthetic block such as a spinal anaesthetic.
Do I have to stay in hospital?
Usually, you stay in hospital for one night after your surgery. However, this can vary based on your health, surgery performed and distance to travel home.
How is the procedure performed?
The hip joint surfaces are separated by about 1cm by placing the whole leg in traction and applying a pulling force. This creates enough space for a small telescope camera to be placed into the joint. X rays are taken and air or fluid injected into the joint. Once the camera is in the correct place 2, 3 or 4 small 5-10mm cuts are made on the side of the hip. These holes allow instruments and the telescope camera to be passed so the surgeon can carry out any treatment. The surgery lasts from 50 – 180 minutes but can be longer than this. Medications can then be injected to provide pain relief. The cuts on the skin surface are then stitched or left open and dressings applied.
What should I expect immediately following the procedure?
It is usual to feel some hip discomfort following the procedure. This discomfort can also affect the lower back, buttock, knee and ankle. Most people have swelling in the groin, buttock and thigh. This reduces over the next few days. It is normal for the wound to leak fluid or blood for a few days. Blood clots in the legs or lungs are rare after the surgery. However, they can be very serious and in very rare circumstances fatal. Unless there are specific contraindications you will be provided with special stocking to wear and up to 4 weeks of blood thinning medication to use to help reduce your risk of developing a blood clot after the surgery.
Is there anything that I should watch out for after the surgery?
Watch out for increasing pain, redness or swelling which are all signs of infection. If this happens contact the ward that you were discharged from.
What will my rehabilitation and physiotherapy involve?
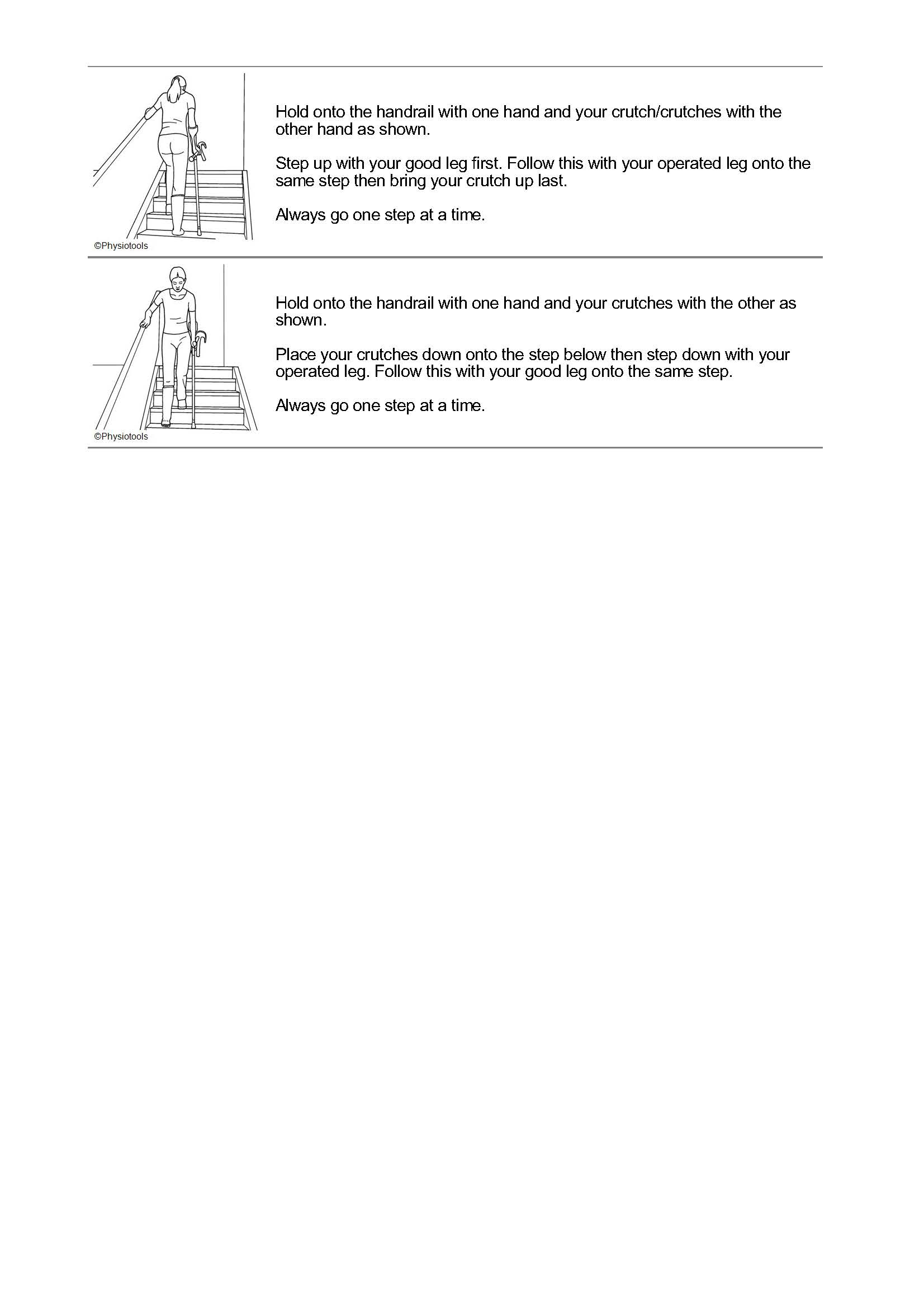
Depending on the nature of the surgery performed on the hip, you will need crutches. This will involve sharing your body weight with the crutches when walking. You will graduate onto 1 crutch and then no crutches. During this time rehabilitation will involve a low-impact exercise programme, and it may also involve hydrotherapy where you will be taught a pool-based exercise programme. Usually, we recommend the use of an exercise bike from 2 weeks after surgery, and the use of a cross-trainer at low resistance can usually start at 4 weeks. The physiotherapist and surgeon will form a rehabilitation plan. The main aims are to regain range of movement and stability as early as possible after which strength and endurance can be regained.
Are there any activities that I should avoid?
In the first 8 weeks after surgery, you should avoid standing on hard surfaces for an extended period, walking for too long, heavy lifting, squatting, crouching and sleeping on your side.
When will I be seen again after my surgery?
A member of the team will usually see you at about 6 to 8 weeks following your surgery. They will answer any questions about your surgery and any further follow up will be decided upon.
When will I be back to normal?
Most people are back to walking relatively pain free by 2 to 3 months after surgery. Athletes should note that it can take about 6 months or even more to return to elite level fitness.
How long will I be off work for?
This depends on your pain level and what your job entails. However, as a rough guide, patients typically are off work for at least 6 weeks so that they can focus on their rehabilitation and exercises.
When can I drive a car?
Your medical team will help guide. However, you should not drive a car until you can safely control the vehicle and do an emergency stop without fear of significant pain around your hip. You should let your car insurance provider know you have had surgery, as they may have specific rules on when you can return to driving. There is also some government guidance on driving after surgery - www.gov.uk/surgery-and-driving.
What painkillers can I take?
Your surgeon or general practitioner will prescribe this for you. Usually, simple paracetamol and ibuprofen is sufficient to manage the pain after you are discharged from hospital.
What about pregnancy?
The operation would be delayed until after the pregnancy.
What are the risks and complications of hip arthroscopy?
The risks of surgery are generally low and permanent complications are rare. The risks are probably in the order of 1-4%. Some of the specific risks are:
Anaesthesia
Modern anaesthetics are very safe. There are some common side effects from the anaesthetic drugs or equipment used which are usually not serious or long lasting. Risk will vary between individuals and anaesthetic technique used. There are other less common risks that your anaesthetist will not normally discuss routinely unless they believe you are at higher risk. A useful resource you may wish to visit is:
www.rcoa.ac.uk/patient-information/patient-information-resources/anaesthesia-risk
Traction
To perform hip arthroscopy traction is applied to the leg. There is a post which applies counter traction in the groin region. As a result, some patients experience numbness or altered feeling in the groin or genitalia region, this can include impotence. This can be permanent although numbness usually recovers within a few weeks. Some patients experience pressure sores and or skin blistering in the thigh or groin region; this may include skin tears, bruising and swelling around the vaginal or scrotal area.
Very rarely despite applying traction to the hip, the joint surfaces will not separate enough to allow safe passage of the telescope and instruments to the joint. If this happens the procedure would need to be abandoned.
Fluid
Fluid is pumped around the hip during the procedure. It is therefore common to get some swelling around the hip and thigh region and for some fluid to leak from the wounds in the first few days after surgery. In very rare circumstances fluid can leak into the abdomen and cause pressure and pain.
Infection
Infection is not common. If this only involves the skin, it can often be treated with a short course antibiotics. However, deeper infection may require further surgery to wash out the joint and an extended period of antibiotics. Severe deep infection is very rare but could damage the joint surface and lead to early onset joint stiffness and arthritis.
Blood clots (deep vein thrombosis and pulmonary embolism)
Blood clots in the leg and lung (so called deep vein thrombosis or pulmonary embolism) are a rare risk of hip arthroscopy. However, if they occur they can be very serious and in some very rare situations fatal. As a result, we take measures to help reduce your risk: including encouraging early mobilisation after surgery and prescribing special stockings and blood thinning medication for up to 4 weeks after the surgery. Patients who are taking the oral contraceptive pill or hormone replacement therapy (HRT) are advised to stop it for at least 6 weeks prior to surgery to help reduce the risk of blood clots.
Nerve and blood vessel injury
Direct injury to major nerves and blood vessels in the leg is very rare but possible. However, some bleeding and bruising around the wound is quite common. In addition, traction related numbness due to pressure on the nerves around the groin is relatively common but usually always recovers within a few weeks.
Other rare events
Other rare risks include damage to the blood supply to the hip (Avascular Necrosis), fracture / break of the hip. Very occasionally the surgical instruments or implants used to perform the surgery break or get damaged within the hip, usually these can be extracted but sometimes they are left as the risks of removing them outweigh the benefits.
What is Hip Impingement or Femoracetabular Impingement Syndrome?
In some people the hip has a subtly abnormal shape and as it moves the abnormally shaped bones press against each other and damage the local soft tissues such as the labrum (a soft cushioning around the hip joint and can cause pain and in the long term is associated with an increased risk of arthritis. The medical term for hip impingement is femoroacetabular impingement syndrome (FAI for short). Hip impingement can affect all age groups. However, it is thought people who do activities that involve a lot of hip movement such as in kicking sports are more prone to getting symptoms.
What are Acetabular labral tears?
The ring of cartilage (labrum) that forms a seal around the hip can become damaged or torn. This is usually associated with either arthritis, hip impingement, previous trauma or direct injury to the hip or dysplasia (a shallow hip). This condition may be diagnosed despite not being seen on an MRI or CT scan as these do not always pick it up. It is not always necessary to do surgery as some are not painful and some heal on their own. However, if it is painful your surgeon may recommend an operation to remove or repair it. If your surgeon thinks you might have dysplasia (a shallow hip) which is causing the labral tear you may need a bigger operation (osteotomy) to help address the problem.
Who can I contact if I have any questions?
Please contact your Consultant Surgeon's secretary.
Where can I find further information?
orthoinfo.aaos.org/en/treatment/hip-arthroscopy/
www.nahr.co.uk/patient-information/
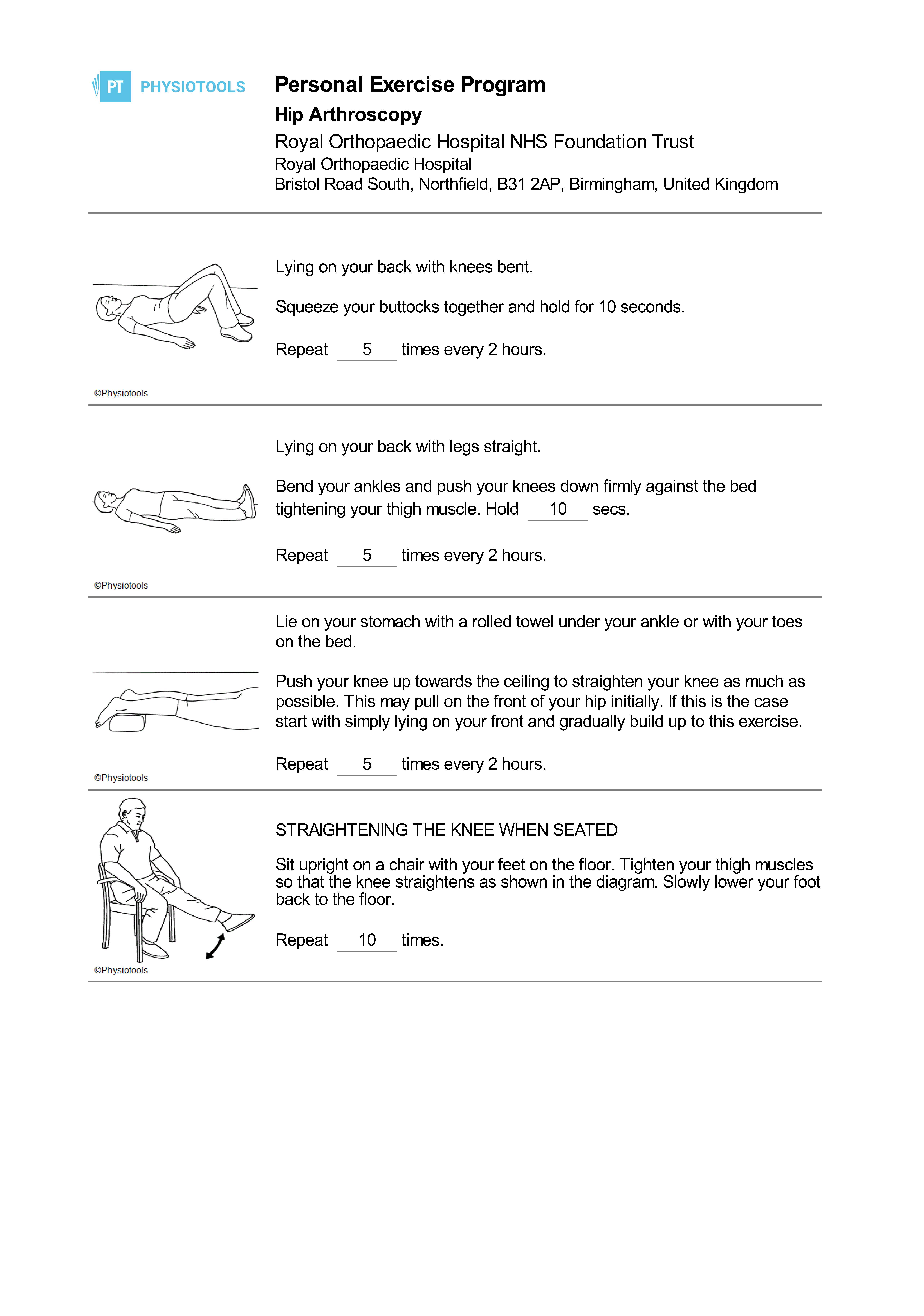
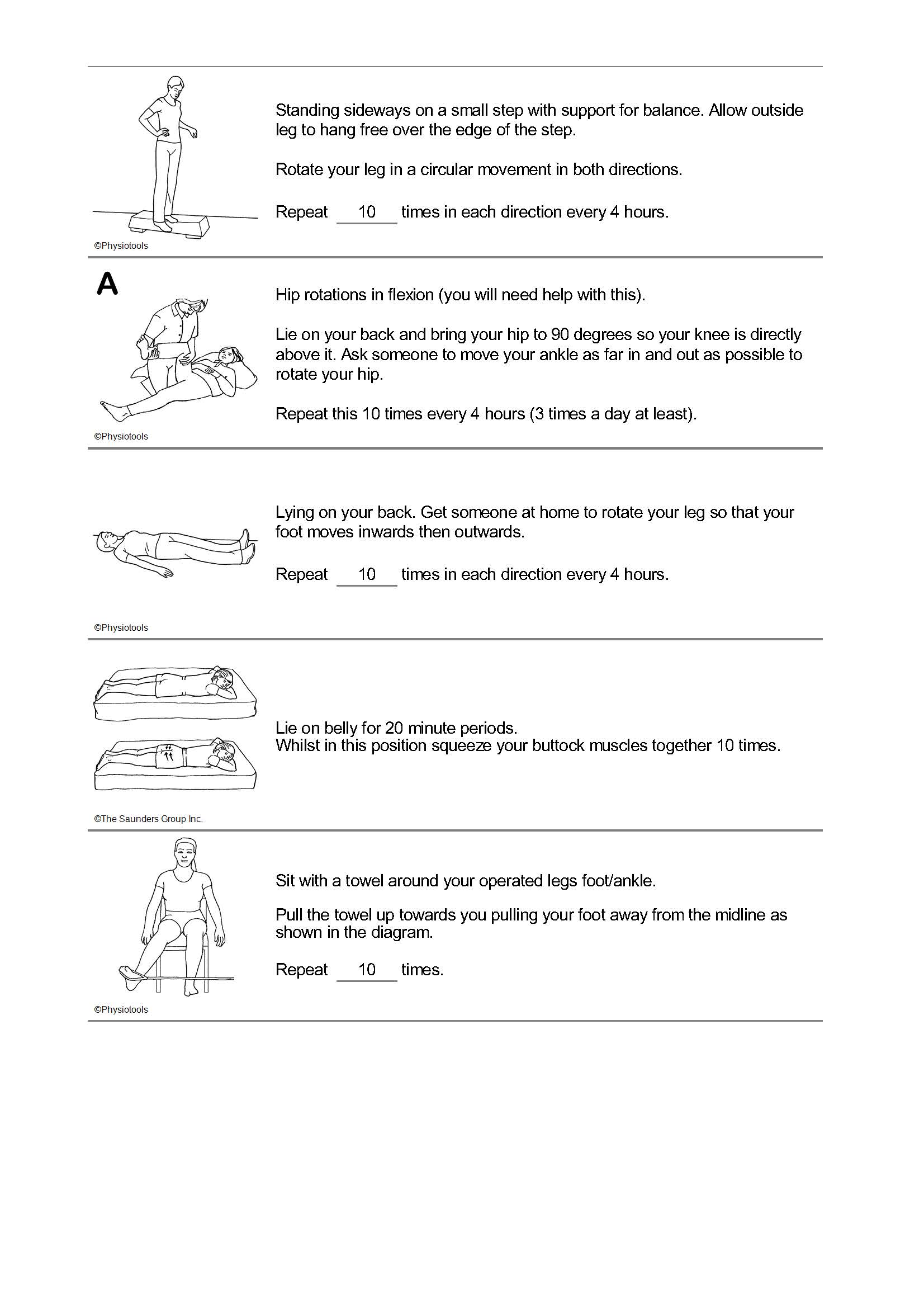
Physiotherapy exercises