
Cubital Tunnel
What is Cubital Tunnel?
Cubital tunnel syndrome is a condition which affects the Ulnar nerve, which is one of the main nerves of your hand. It causes pins and needles, numbness and sometimes pain along your ring and little fingers. You may also have weakness of the hand and in severe cases clawing, curling up, of the ring and little fingers.
What causes Cubital Tunnel Syndrome?
In most cases there is no obvious reason for cubital tunnel syndrome. There are ligaments and fascia (strong fibrous tissues) over the nerve at the elbow, some of which can get tighter and press on the nerve. Sometimes this condition can develop following healed fractures of the elbow when the nerve is stretched behind the elbow prominence.
Your GP or surgeon may arrange a test called a Nerve conduction study to confirm the diagnosis. Your GP or surgeon may have arranged a test called Nerve conduction study to confirm the diagnosis. This test is not always sensitive at picking up this problem. Even if the test is negative, you may still be having cubital tunnel syndrome. The test however can give an indication about the severity of the condition and also diagnose other conditions which may be confused with this.
What treatments are available for this condition?
Surgery
The operation is meant to relieve the pressure of the nerve and by doing so, you should get improvement in the pins and needles in the fingers. You may also get improvement in the strength in the small muscles of the hand. This improvement may be instant or gradual over 12-18 months. In cases of advanced compression, the nerve may not recover fully even after release and in those cases, surgery prevents further damage.
Treatment for Cubital tunnel syndrome is a worthwhile operation which usually relieves your symptoms if they are intermittent and will improve them to some extent in more severe cases. Treatment can improve your hands function and reduce the stress and sleep interference of symptoms.
Postural adaptation
In some cases, postural adaptations by avoiding prolonged periods with the elbow bent may help to relieve the symptoms. Splinting the elbow at night may help some people but is often poorly tolerated. Some patients may choose to live with the pins and needles and opt not to have an operation.
What happens on the day of surgery?
Admission
On the day of surgery, you will be admitted by a nurse who will check your details, medications and past medical conditions and put a wrist band with your details on the arm is not being operated on (if we are operating on both hands this band is put on your ankle).
Remove any rings before you come to hospital and if you are unwell or have any cuts on your hand or arm then please inform us before the day as this may require your operation to be delayed.
Anaesthetic
The anaesthetic options are a general anaesthetic where you go to sleep or an axillary block with or without sedation (this is where you are awake but have a numbing injection in your armpit and the whole arm is numb for 12 hours).
If you have an axillary block, this takes 20-30 minutes to work and therefore you will spend this time waiting in the anaesthetic room. Both the anaesthetist and surgeon will check the arm is fully numb before surgery. If you are having a brachial block and are awake during the operation, you may feel a cuff over the top of the arm. This is called a tourniquet and is to stop the blood flow into your arm during the operation. You may sometimes feel the tightness from it being inflated but if it is uncomfortable, you should let one of the team know.
If you are staying awake for your surgery, there is the option to listen to music or watch a video on the tablet screens and headphones we have in theatre. Alternatively, you can bring your own device to listen to music on, but you must have headphones.
Depending on what anaesthetic you have, you may have to starve for your surgery. You will be advised before your admission whether you will have to starve or not.
Surgery
Surgery time varies from 20-60 mins depending on the complexity of the surgery, your surgeon will be able to tell you about the rough operative time on the day of surgery. Once your arm is cleaned and draped, the surgeon will make an incision over your elbow and release the tight structures on top of the nerve. Once the nerve is fully released, the surgeon will check if the nerve is unstable or too tight behind the elbow by bending your elbow. In both these cases a simple decompression may not relieve your symptoms. If that is the case, you may need another procedure called a ‘nerve transposition’ or ‘medial epicondylectomy’. Your surgeon should have discussed the possibility of this with you during the consenting. In recurrent cases one of these options may have already been planned as the procedure to be carried out. A nerve transposition is carried out by moving the nerve from the back to the front of the elbow. The nerve may be placed under the skin or under the muscle depending on the surgeon’s preference. This allows the nerve to take a ‘short cut’ to prevent it being stretched behind the elbow when it is bent. A medial epicondylectomy is an alternative procedure where the medial epicondyle or the tip of the ‘funny bone’ is shaved down to relieve the tension on the nerve.
Once the operation is complete the wound is closed, and your arm is bandaged. You will be given a sling to keep the arm elevated. You may go back to ADCU straightaway or sometimes sent to the recovery for one hour if you have had a general anaesthetic.
After surgery
The Nursing team will make sure that you are sufficiently recovered from the operation before you are allowed home. You should have someone to take you home and be with you overnight after the operation. Almost all patients will go home on the day of surgery. Very occasional, social or medical conditions require an overnight stay.
What are the possible complications from this operation?
Whilst the surgical team makes sure that the operation is carried out with utmost safety, complications may still happen. Your surgeon should have discussed these with you. The percentage values given cover a range from simple to complex cases. There are risks with the anaesthesia and your anaesthetist will discuss them with you.
- Bleeding - as this operation is carried out under a tourniquet, bleeding may happen after the operation is finished causing marked bruising and wound oozing (15%). Very rarely if a blood clot collects under the skin, you may need an operation to remove it and stop the bleeding.
- Infection – this is rare (2-19%) following this operation but if it happens, you may need to have antibiotics. In very rare cases another operation.
- Scar - the scar behind the elbow usually fades well but, in some people, it can be more prominent (10-13%).
- Pain - the scar will be tender for at least four to six weeks and in some cases such as with anterior transposition and medial epicondylectomy (15-52% have pain) the pain may take 2-3 months to settle around and deep to the scar. Occasionally patients feel pain or abnormal in their fingers after surgery where it has been numb before. This usually subsides as the nerve starts to recover although may take 2-3 months.
- Nerve injury - there is a small risk of injury to the nerves in the skin around the scar (1%). If this happens you may have a numb patch of skin on your inner arm and sometimes can have a painful spot in the arm. Often there is some numbness over the scar line in a very small area which doesn’t cause any issues (11-32%). The risk of injury to the main nerve is extremely rare and if it happens you may have permanent numbness to your fingers and weakness to your hand.
- Nerve instability – occasionally once the nerve is released it becomes unstable and flicks over the bony part of the elbow as it is bent. This can cause tingling and numbness. If this is seen during surgery a transposition or epicondylectomy will be performed. This rarely happens following surgery and may need reoperation (4%).
- Continued symptoms - your symptoms usually improve within three to four weeks after the operation but in some cases, often those with more severe nerve damage, it may not improve. There is a small risk that the symptoms may be worse due to dissection around the nerve. Occasional further surgery may be required if symptoms persist (6-13%)
- Complex regional pain syndrome - very rarely you can develop a condition called complex regional pain syndrome (CRPS) (less than 1%) which can make your hand red, swollen and painful. This is a difficult condition to treat and may last for several years. Treatment consists of pain killers and Hand therapy.
- Elbow instability – rarely during a medial epicondylectomy the supporting ligament around the elbow can be injured requiring further surgery (1-10%).
What should I do about my medication?
Let the doctor know about your medication in the clinic. For all procedures you will be seen in the preassessment clinic before surgery who will advise exactly what to do regarding any medications which you will need to reduce or stop.
How do I make my operation a success?
- If you smoke it is best to stop or reduce as much as you can. If you are diabetic, you will reduce your risk of infection and poor wound healing by keeping your blood sugars stable.
- Please attend all dressing, doctor and hand therapy appointments after surgery and follow instructions on hand exercises to get the best function and recovery following surgery.
What happens after surgery?
Once you are home you need to rest and elevate your hand in the sling for 48 hours. You may be able to use your hand for light activities (dressing etc.) after that. The bulky bandage will make it difficult to wear normal clothes and you may need to wear a loose short sleeved top or T-shirt. If you are having a shower you will have to put a waterproof plastic bag to cover the bandage.
The dressings will be changed between five and seven days in the clinic. You may be able to do more things using your hand at this stage and if the stitches are dissolvable ones, you can even get it wet.
The appointments after this will depend on your recovery at the initial review. Once fully recovered you will be discharged.
How long will it take to recover?
You can drive when your wounds are healed, and you feel you can safely grip the steering wheel in both hands to control the car. This usually takes 2-3 weeks. Any heavy physical work may be possible only after six weeks.
You can shower or bath as normal once the wounds are healed, but prior to that you need to keep the hand dry. If you have any issues such as elbow or scar pain, we will arrange for you to see the Hand Therapist who will help.
The symptoms usually improve gradually and over the six weeks you should be experiencing improvements in the symptoms. If your symptoms fail to improve your surgeon will assess you during the next appointment and advise you.
What happens if I decide to not have surgery?
In mild cases where there is no weakness or permanent numbness the symptoms may improve on their own without surgery. If your symptoms are not severe it is not unreasonable to wait and see if they get better.
If symptoms are severe meaning the numbness is there all the time or there is weakness in the hand, then not treating it is likely to lead to a worsening of symptoms and hand function. The longer the nerve is squashed for and the more severe the symptoms the less likely the nerve will make a full recovery once released. Once muscles become thinned and very weak, they are unlikely to recover despite surgery.
After surgery information
- Elevate your hand in a sling whilst mobilising and on a pillow when sitting or in bed.
- Do not allow your hand to hang down by your side.
- Keep the dressing dry, try not to disturb the dressing until you have been advised to.
- Do not partake in heavy manual work until you have been seen at your next appointment and have been advised it is safe to do so.
- Take painkillers as prescribed.
- If you are instructed to wear a sling, please ensure you remove your arm from the sling every 1 to 2 hours and exercise the shoulder and elbow to prevent them from getting stiff. Remember to also wriggle your fingers.
If you experience pain, numbness, tingling, excessive swelling, discharge through your dressing or discoloration of the fingers, in the first instance please contact the Outpatients Department (Mon - Fri, 8:30am - 4:30pm).
Outside of these hours, please contact the main hospital number and ask for the Clinical Site Co-Ordinator on call: 0121 685 4000.
If you are unable to make your Outpatient appointment, please contact the Appointments department on 0121 812 3200.
Post-operative exercises
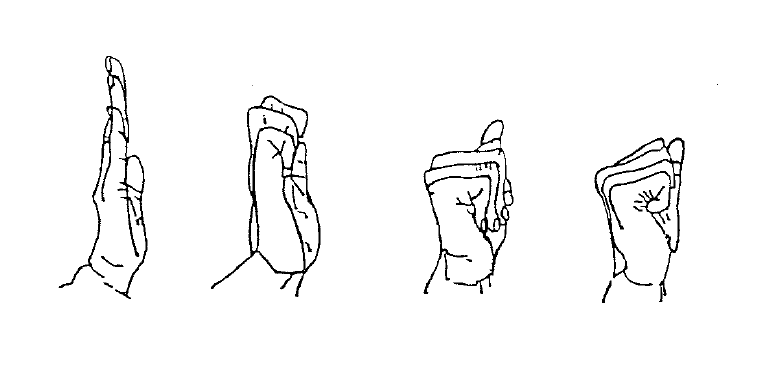
Finger Exercises
Starting from a straight position, do 10 repetitions of each type of fist shown
Therapy information

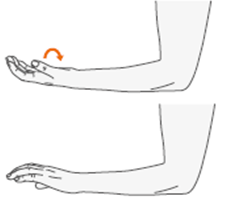
Elbow bend
- Stand up straight and lower your arm to one side
- Bend your arm slowly upwards so your hand is touching your shoulder
- Hold for 15-30 seconds

Ulnar nerve mobilization
- Stand up comfortably.
- Start with your hand down at your side.
- Lift your hand up sideways to bring it over your ear.
- Rotate the hand so the fingers point downward when against your ear.
- To increase the tension, you can push your elbow backward at the end.
- Do not execute the exercise too fast; the symptoms can arise quickly. Stop the movement at the edge of where your symptoms are reproduced.