Trapeziectomy
What is the Trapezium?
The Trapezium is a small wrist bone that lies at the base of your thumb. It is commonly affected by wear and tear, otherwise known as arthritis.
How does arthritis happen?
Arthritis affecting this bone is very common. It can be related to age, activity, injury or can be inherited. With time the joint becomes worn. Progressively it leads to increasing pain, weakness in grip, stiffness and eventually it may cause deformity at the base of the thumb.
Initially, the symptoms may be related to certain activities such as opening jars and strong gripping. As the condition progresses, the symptoms can become more pronounced and permanent.
What is a Trapeziectomy?
It is the removal of this bone.
What are the benefits of surgery?
Surgery gives the best chance of reducing your pain. This may consequently improve your hand function.
What are the treatment options?
Non surgical
There are several non-surgical treatments available depending on how severe your symptoms are. You can avoid certain activities that cause you pain or take painkillers. Your hand therapist can provide or make splints for you to rest your thumb in. Your doctor may also inject the joint with steroid (cortisone). This can be done under ultrasound or X-ray guidance usually on a different day from the outpatient appointment. The injection only provides temporary relief of symptoms (3-6 months) or may not be successful at all. Repeated injections often last a shorter duration each time. They do not cure the condition.
Surgical
There are four different surgical options:
- Trapieziectomy – this is where the bone is removed completely. The gap fills with scar tissue on which your thumb will sit to reduce the pain of the bone on bone rubbing. 85% of patients have a significant pain improvement.
- Trapeziectomy with tendon sling – the bone is removed and part of a tendon of your thumb or wrist is used to wrap around the thumb bone and roll up into the gap to support the thumb during healing (you will not notice a functional problem by loss of your tendon). No clear advantage is shown comparing this option with simply removing the bone in most cases.
- Joint fusion – a screw, plate or staple is placed across the joint to stiffen it and stop the bone on bone rubbing which causes pain. Often reserved for young manual laborers.
- Joint replacement – like a hip or knee, some surgeons replace the joint in very specific patient cases.
What happens on the day of surgery
Admission
On the day of surgery, you will be admitted by a nurse who will check your details, medications and past medical conditions and put a wrist band with your details on the arm we are not operating on (if we are operating on both hands this band is put on your ankle).
Remove any rings before you come to hospital and if you are unwell or have any cuts on your hand or arm then please inform us before the day as this may require your operation to be delayed.
Anaesthetic
You must starve for your surgery as you may have a general anaesthetic where you go to sleep, or an axillary block (this is where you are awake but have a numbing injection in your armpit and the whole arm is numb for 12 hours), this block can be done with or without sedation. You must not eat, drink or chew gum for 6 hours before you come to hospital. Up to 2 hours before you can drink clear water only.
You will be seen by the anaesthetist who will check your current health, ask specific questions about medications and when you have last eaten or drank. They will then discuss the details of the anaesthetic including the process, risks and answer any questions you have. They will then mark your arm with an ‘A’ if you are having an axillary block.
If you are staying awake for your surgery, there is the option to listen to music or watch a video on the tablet screens and headphones we have in theatre. Alternatively, you can bring your own device to listen to music on, but you must have headphones.
If you have a general anaesthetic, the next thing you will remember is waking up in recovery after the surgery. If you have an axillary block, this takes 20-30 minutes to work and therefore you will spend this time waiting in the anaesthetic room. Both the anaesthetist and surgeon will check the arm is fully numb before surgery.
Surgery
Before the procedure you will be seen by one of the surgical team who will go over your procedure, consent form and answer any questions about the surgery or recovery. They will then draw a mark on the arm you are having on operation on.
When it is your turn to go to theatre you will be asked to change into a theatre gown and walk with a member of the theatre team or porter to the theatre if able.
Surgery time varies from 30-90 mins depending on the specific surgery being undertaken. Your surgeon will be able to tell you about the rough operative time on the day of surgery.
Your surgeon will make a cut a few centimeters long over the trapezium either on the back or the palmar side of your hand. They will carefully isolate the bone before removing it. The wound will be closed with stitches. You will have a plaster cast or a bulky dressing around your thumb at the end of the procedure, and an arm sling to elevate your hand.
After surgery
You will go back to ADCU unless you have had a general anaesthetic. If you have had a general anaesthetic, you will go to recovery for one hour before you return to ADCU.
Once you are back in ADCU the nurses will make sure that you are sufficiently recovered from the operation before you are allowed home. You should have someone to take you home and be with you overnight after the operation.
Almost all patients will go home on the day of surgery. Very occasional, social or medical conditions require an overnight stay.
Going home after surgery
You will go home on the same day and return to a dressing clinic, usually a week or 2 later, to assess your wounds and remove the plaster if present. At this point depending on the specific type of operation you have had you may go into a splint or back into plaster cast until 6 weeks after surgery. You will start exercises with the hand therapist if required. The appointments after this will depend on your recovery at the initial review.
You can shower or bath as normal once the wounds are healed if you have a removal splint. If you have a plaster, you need to keep the hand and plaster cast dry until it is removed.
Once fully recovered you will be discharged if your other thumb is not causing any issues. If you are part of a trial, additional appointments may be required however you will be clearly notified of this. If you are worried about anything in hospital or at home, please contact the healthcare team. They should be able to reassure you or identify and treat any complications.
What are the possible complications?
The healthcare team will try to make the operation as safe as possible, but complications can happen. Some of these can be serious. You should ask your doctor if there is anything you do not understand. The statistical figures which relate to risk are from studies from people who have had this operation. Your doctors may be able to tell you if the risk of a complication is higher or lower for you.
There are also risks with the anaesthesia and your anaesthetist will discuss them with you.
The % values given cover a range from simple to complex cases.
- Bleeding - during or after surgery. This generally stops by itself. The risk of bleeding is higher in patients who are on blood thinning medications and your doctor will advise on when to stop them before the operation to reduce the risk. Injury to an artery near the base of thumb is possible but if identified in surgery is unlikely to cause any noticeable problems.
- Pain - take regular painkillers for at least a week. The healthcare team may give you additional pain medications. It is important that you follow the instructions so you can do hand exercises as advised.
- Infection - the risk of the wound becoming infected is less 1-22%. Your wound will be reviewed in the dressing clinic. Inform the healthcare team if you have a temperature, have ‘increasing’ pain or swelling beyond 3 days or notice any smell from the dressings.
- Scarring - this can be tender or unsightly (3-20%). Your healthcare team will teach you how to massage and soften your scar as it heals.
- Skin nerve damage - damage to a small skin nerve may lead to a tender scar or numbess over the back of the hand between the thumb and first finger. (3-16%)
- Continued pain or weakness - (36%) this may be mild or rarely similar to before the operation. It can be caused by the thumb bone sinking down a little, surrounding arthritis, pain from where the tendon was taken 10-19% (if used) and may require further surgery in 10% of patients.
- Complex regional pain syndrome – pain, stiffness, and loss of use of your hand (2-8%) The exact cause remains unknown. This varies in severity and is treated by means of painkillers and physiotherapy. It may take weeks and months to improve.
- Tendon problems – if a tendon was used to support the thumb it can snap or move position which may lead to increased pain in 1-4% of patients.
- Carpal instability – in 50-67% of patients the removal of one bone allows the other to lean or move slightly out of place. This is unlikely to cause noticeable problems but will rarely cause pain and a decreased grip strength.
What should I do about my medication?
Let the doctor know about your medication in the clinic. For all procedures other than local anaesthetic procedures you will be seen in the preassessment clinic before surgery who will advise exactly what to do regarding any medications which you will need to reduce or stop.
What can I do to make the operation a success?
If you smoke it is best to stop or reduce as much as you can. If you are diabetic, you will reduce your risk of infection and poor wound healing by keeping your blood sugars stable.
Please attend all dressing, doctor and hand therapy appointments after surgery and follow instructions on hand exercises to get the best function and recover following surgery.
How quickly will I recovery from surgery?
The scar will be red and raised initially which generally settle with time. You cannot drive until you feel you can safely grip the steering wheel in both hands to control the car. This is normally 6 weeks at the earliest. Heavy lifting is not recommended until 3 months after surgery. Grip strength and pain can continue to improve up to 1 year after surgery. Occasionally pain may persist due to other causes. If it is a problem this can be investigated and reviewed by your surgeon.
What would happen if I decided not to have surgery?
You may wish to try non-surgical options first. It does not stop the progression of your arthritis. If these treatments are not affective, you may wish to consider surgery. If you do not have surgery your pain and disfunctions are likely to continue but in some cases the joint actually becomes stiffer and less painful with time.
After surgery information
- Elevate your hand in a sling whilst mobilising and on a pillow when sitting or in bed.
- Do not allow your hand to hang down by your side.
- Keep the dressing dry, try not to disturb the dressing until you have been advised to.
- Do not partake in heavy manual work until you have been seen at your next appointment and have been advised it is safe to do so.
- Take painkillers as prescribed.
- If you are instructed to wear a sling, please ensure you remove your arm from the sling every 1 to 2 hours and exercise the shoulder and elbow to prevent them from getting stiff. Remember to also wriggle your fingers.
If you experience pain, numbness, tingling, excessive swelling, discharge through your dressing or discoloration of the fingers, in the first instance please contact the Outpatients Department (Mon - Fri, 8:30am - 4:30pm).
Outside of these hours, please contact the main hospital number and ask for the Clinical Site Co-Ordinator on call: 0121 685 4000.
If you are unable to make your Outpatient appointment, please contact the Appointments department on 0121 812 3200.
Post-operative exercises
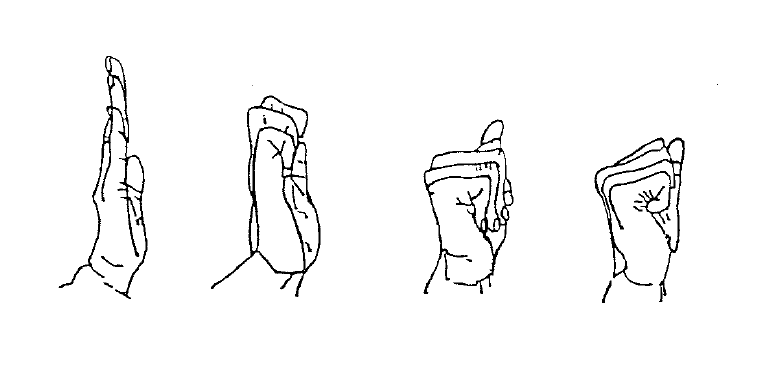
Finger Exercises
Starting from a straight position, do 10 repetitions of each type of fist shown.