Trigger Finger / Thumb
What is trigger finger?
Trigger finger is a condition that causes the finger to ‘catch’ or ‘click’ or ‘trigger’ when it is bent and straightened. It can affect more than one finger, and when it involves the thumb, it is known as trigger thumb. The condition initially develops as a small tender fullness in the palm in line with the finger or thumb. This then progresses to triggering or catching, associated with varying degrees of stiffness and increased pain. In severe cases the finger becomes held bent into the palm or is unable to fully straighten.
What causes trigger finger?
The flexor tendons (the ropes that bend your fingers and thumb) pass through narrow tunnels in the palm and fingers known as pulleys. Occasionally the tendons or tunnels become thickened. When thickening occurs, the finger begins to catch. With further thickening it may become stuck bent into the palm. It is a common condition, but there is a higher risk of developing it in women, diabetic patients and people with occupations that require repetitive gripping movements. Most commonly no medical cause is identified although the thickening may be related to diabetes or rheumatoid arthritis.
What treatment options are available?
Non-surgical
There are various non-surgical treatments available. Some patients modify their activities, whereby they reduce or stop the repetitive gripping movements that cause triggering.
- Non-steroidal pain killers such as Ibuprofen can reduce the discomfort associated with the inflammation, however this will not necessarily prevent the triggering effect.
- Splinting of the finger in a straight position prevents the tendons from gliding through the thickened pulleys, and hence stops triggering. These splints can be custom-made by the hand therapists in the outpatient clinic and are only worn at night to allow the swelling around the tendon to settle over time.
- A steroid (cortisone) injection into the base of the finger or thumb is preferred by most patients as the first-line treatment. It is usually combined with a local anaesthetic (Lidocaine) and the procedure is performed by the doctor in the outpatient clinic. The steroid reduces inflammation. It can resolve pain and triggering in 70-80% of patients. It is less effective in diabetic patients, those with multiple trigger fingers, and severe cases with long-standing symptoms. The procedure can be repeated, although are less effective with each subsequent injection.
Surgery
Surgery is offered if non-operative methods have not worked. There are two types: percutaneous and open surgery. The percutaneous technique involves inserting a needle through the skin into the sheath and using the tip of the needle to cut open the roof of the sheath. With the more common open technique, a cut (incision) is made at the base of the finger. This creates a better exposure for cutting the pulley.
Surgical release for trigger finger is a worthwhile operation which has good results. Treatment can improve your hand function and resolve the pain and catching whilst bending and straightening the fingers. It is generally safe but complications, though uncommon, can happen.
What are the benefits of treatment?
The aim of treatment is to reduce pain and allow the fingers to bend and straighten without triggering and ultimately restore hand function.
What happens on the day of surgery?
Admission
On the day of surgery you will be in ADCU (Admission and Day Case Unit) you will be admitted by a nurse who will check your details, medications and past medical conditions and put a wrist band with your details on the arm we are not operating on (if we are operating on both hands this band is put on your ankle).
Remove any rings before you come to hospital and if you are unwell or have any cuts on your hand or arm then please inform us before the day as this may require your operation to be delayed.
Anaesthetic
In the vast majority of cases, you will have a local anaesthetic where the injection is in your hand and just part of your hand goes numb. Rarely in the case of multiple fingers or revision surgery you may require the whole arm to be numbed or opt for sedation or general anaesthetic (to go to sleep). Your surgeon will discuss these options with you during the consent process and also advise you if you are required to starve or not prior to the procedure.
If you are having a general or axillary block anaesthetic you will be seen by the anaesthetist who will check your current health, ask specific questions about medications and when you have last eaten or drank. They will then discuss the details of the anaesthetic including the process, risks and answer any questions you have. They may then mark your arm with an ‘A’ if you are having an axillary block.
If you are having a local anaesthetic, the surgeon will then inject anaesthetic into your hand and if required a tourniquet will be put on your arm. This is to stop the blood flow in the arm while the operation is taking place. It is a tight band around the top of your arm similar to having your blood pressure taken.
If you are having an axillary block or a general anaesthetic, your details will be checked again, and the anaesthetist will perform the anaesthetic. If you have an axillary block, this takes 20-30 minutes to work and therefore you will spend this time waiting in the anaesthetic room. Both the anaesthetist and surgeon will check the arm is fully numb before surgery.
If you are staying awake for your surgery, there is the option to listen to music or watch a video on the tablet screens and headphones we have in theatre. Alternatively, you can bring your own device to listen to music, but you must have headphones.
Depending on what anaesthetic you have, you may have to starve for your surgery. You will be advised before your admission whether you will have to starve or not.
Surgery
You be seen by one of the surgical team who will go over your procedure, consent form and answer any questions about the surgery or recovery. They will then draw a mark on the arm you are having the operation on.
Once the hand is numb, the surgeon makes an incision at the base of the finger and cuts the roof of the pulley sheath. Afterwards the skin is sutured, and a bulky dressing is applied to protect the wound. Surgery time usually varies from 10-30 mins depending on the number of digits operated on.
After surgery
You will return to ADCU after the surgery. If you have had a general anaesthetic you will go to recovery before returning to ADCU. The nurses will make sure that you are sufficiently recovered from the operation before you are allowed home. You should ideally have someone to take you home and be with you overnight after the operation. Almost all patients will go home on the day of surgery. Very rarely, social or medical conditions require an overnight stay.
What are the possible complications from this operation?
Minor complications are uncommon in trigger finger surgery, whilst significant complications are even more rare. However, the more severe the disease and the more procedures have taken place before on the finger, the increased likelihood of a complication. Diabetic patients also have a higher risk of complications.The percentage values given below are estimates based on previous clinical studies in the medical literature. There are risks with the anaesthesia, and your anaesthetist will discuss them with you.
- Pain – when operating on more than one finger at a time the patient may experience more pain and this can occasionally last longer than anticipated. We no longer provide anti-inflammatory medication or Paracetamol as they are available over the counter. If we feel stronger pain killers are required they will be given to you on the day to take home. Scars may be tender for a number of months in 10% of patients.
- Stiffness – patients who have long-standing trigger finger, or have multiple digits operated on are at higher risk of stiffness (approximately 15%).
- Chronic regional pain syndrome – this is a very rare condition but can happen in patients with more extensive surgery. There is increased pain and stiffness in the hand which may last many months and is treated with pain killers and physiotherapy.
- Bleeding – most wounds ooze a little and the dressing will usually soak this up and be fine until you are seen in a dressing clinic. Rarely there is increased bleeding which may soak the dressings. In this case please urgently contact the hospital and return for a change of dressing and review.
- Infection and wound breakdown – infections occur in 2% of cases although it is extremely rare to need further surgery. A course of antibiotics will normally cure the infection. The wound will be reviewed in the dressing clinic after surgery to assess for any healing issues or any infection
- Nerve and/or arterial injury – bruising or cutting of a nerve can lead to a temporary or permanent loss of sensation in half or all of the finger. This is rare in a primary procedure but occurs slightly more frequently if previous operations have taken place on the finger. There is also a possibility of nerve injury if having an axillary block. Temporary tingling or numbness occur in 1 in 100 patients with permanent problems in 1 in 3000 patients. Similarly, arterial injury is very rare. As there are two arteries in the finger, damage to one of them is extremely unlikely to lead to amputation of the finger but the digit can become sensitive or painful in cold weather.
- Tendon issues – in complex cases the tendon that moves the finger may be cut or the tendon may appear more prominent when attempting to bend the finger (known as ‘bowstringing’). The risk of these occurring is roughly 1%.
- Recurrence of triggering - despite cutting the pulley, scar tissue can develop internally, re-creating a thickening that prevents smooth tendon gliding. This can occur in 2%, requiring a repeat or ‘revision’ procedure.
What should I do about my medication?
Let the doctor know about your medication in the clinic. If you are having a general anaesthetic, sedation or axillary block you will be seen in the pre-assessment clinic before surgery and you will be advised exactly what to do regarding any medications that need to be reduced or stopped.
What happens after my surgery?
Once you are home you need to rest and elevate your hand in the sling for 24-48 hours. You may be able to use your hand for light activities (dressing etc.) after that. The bulky bandage will make it difficult to wear normal clothes and you may need to wear a loose short sleeved top or T-shirt.
If you are having a shower you will have to put a waterproof plastic bag to cover the bandage.
The dressings will be changed between five and seven days in the clinic. You may be able to do more things using your hand at this stage and if the stitches are dissolvable ones, you can even get it wet. Dissolvable stitches start to fall out when washing your hand between 2-3 weeks. If non-dissolvable stitches were used, we will arrange to remove them either in the clinic or at your GPs.
The appointments after this will depend on your recovery at the initial review. You may be referred to a hand therapist for finger movement and strengthening exercises.
What can I do to make the operation a success?
If you smoke it is best to stop or reduce as much as you can. If you are diabetic you can reduce your risk of infection and poor wound healing by keeping your blood sugars stable.
Please attend all dressing, doctor and hand therapy appointments after surgery and follow instructions on hand exercises to get the best function and recover following surgery.
How quickly will I recover from the surgery?
You can drive when your wounds are fully healed and you feel you can safely grip the steering wheel with both hands to control the car. This usually takes 3 to 4 weeks. Any heavy physical work may be possible only after 6 weeks.
You can shower or bath as normal once the wounds are healed, around 10 days post surgery or when the stiches are removed but prior to this you need to keep the hand dry.
Once fully recovered you will be discharged if no other fingers are causing issues. If you are part of a clinical trial, additional appointments may be required however you will be notified of this.
After surgery information
- Elevate your hand in a sling whilst mobilising and on a pillow when sitting or in bed.
- Do not allow your hand to hang down by your side.
- Keep the dressing dry, try not to disturb the dressing until you have been advised to.
- Do not partake in heavy manual work until you have been seen at your next appointment and have been advised it is safe to do so.
- Take painkillers as prescribed.
- If you are instructed to wear a sling, please ensure you remove your arm from the sling every 1 to 2 hours and exercise the shoulder and elbow to prevent them from getting stiff. Remember to also wriggle your fingers.
If you experience pain, numbness, tingling, excessive swelling, discharge through your dressing or discoloration of the fingers, in the first instance please contact the Outpatients Department (Mon - Fri, 8:30am - 4:30pm).
Outside of these hours, please contact the main hospital number and ask for the Clinical Site Co-Ordinator on call: 0121 685 4000.
If you are unable to make your Outpatient appointment, please contact the Appointments department on 0121 812 3200.
Post-operative exercises - Trigger Finger
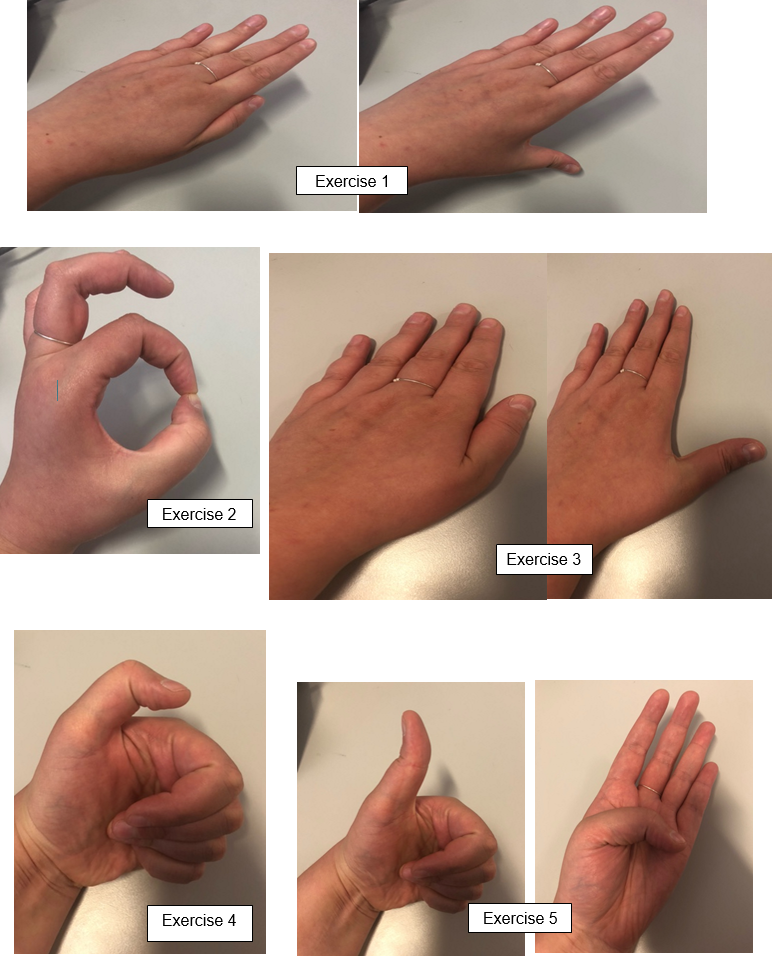
Finger Exercises
Starting from a straight position, do 10 repetitions of each type of fist shown.
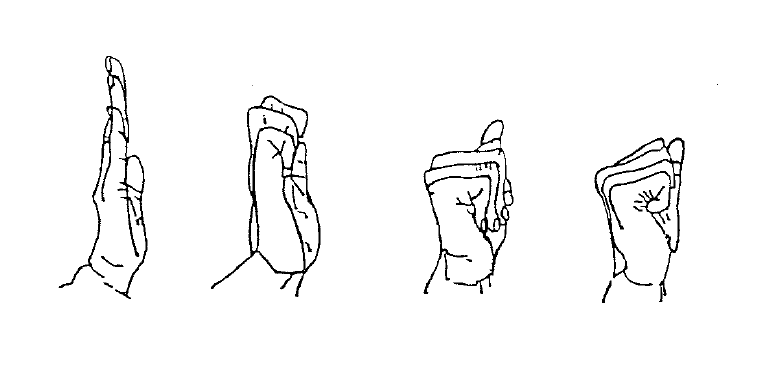
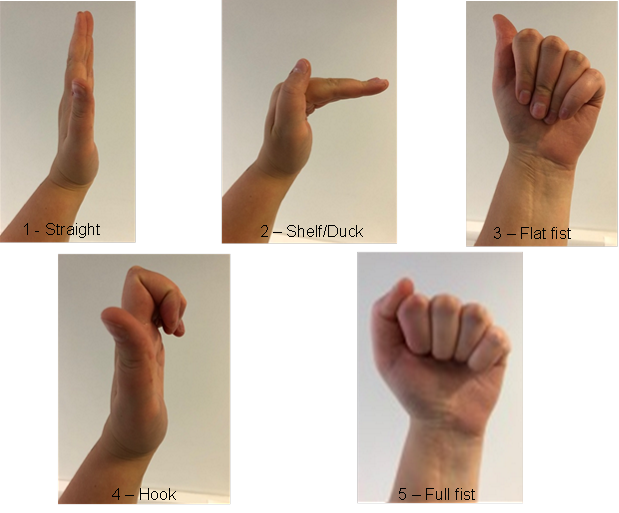
Trigger Thumb